Servicios Personalizados
Articulo
Indicadores
Compartir
SMAD. Revista eletrônica saúde mental álcool e drogas
versión On-line ISSN 1806-6976
SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. (Ed. port.) vol.16 no.1 Ribeirão Preto enero/mar. 2020
http://dx.doi.org/10.11606/issn.1806-6976.smad.2020.156687
ORIGINAL ARTICLE
Epidemiological profile of the users of a Psychosocial Care Center
Camila Gomes BarbosaI ; Paulo Roberto Marinho MeiraI
; Paulo Roberto Marinho MeiraI ; Joilda Silva NeryII
; Joilda Silva NeryII ; Bruno Bezerra GondimI
; Bruno Bezerra GondimI
IUniversidade Federal do Vale do São Francisco, Departamento de Medicina, Paulo Afonso, BA, Brazil
IIUniversidade Federal da Bahia, Departamento de Saúde Coletiva, Salvador, BA, Brazil
ABSTRACT
OBJECTIVE: to analyze the clinical and sociodemographic characteristics of users of the Psychosocial Care Center II (CAPS II) in the city of Paulo Afonso - Bahia.
METHOD: this is a quantitative and cross-sectional study, conducted from the survey of data from patients attending CAPS II of Paulo Afonso, in 2018. Clinical and sociodemographic aspects were obtained from the medical records of the active users of the service whose years of registration ranged from 2006 to 2018.
RESULTS: prevailed female gender, single marital status, incomplete elementary school and illiteracy, age between 40 and 49 years, employed persons, non-intensive care and admission by referral. The most frequent diagnosis was in the group of schizophrenic, schizotypic and delusional disorders. The diagnoses were significantly associated with the variable "gender", being the male gender with higher prevalence of disorders in the groups of organic mental disorders, schizophrenia, schizotypic and delusional disorders and mental retardation. The female had a higher proportion in mood disorders and neurotic disorders related to stress and somatoforms.
CONCLUSION: the data obtained in this study are relevant to contribute to the direction of improvement strategies and organization of the Paulo Afonso Psychosocial Care Center.
Descriptors: Mental Disorders; Epidemiological Profile, Psychosocial Care Center.
Introduction
Mental disorders are syndromes that interfere with biological and psychological processes fundamental to the emotional, cognitive and behavioral regulation of individuals. Thus, they relate to the suffering and impairment of activities of the personal and working life of those affected(1). These disorders deserve attention as they affect millions of people worldwide and have high levels of discrimination, early death and physical and sexual abuse(2). It is estimated that of four individuals, one will be affected by mental disorders at some point in life(3). Thus, it is important that the mental health network be prepared to adequately host and treat its patients.
For a long time, however, assistance was restricted to the asylum model, which focused on long-term hospitalizations in psychiatric hospitals where abuse was recurrent. In order to change this scenario in Brazil, the Brazilian psychiatric reform was instituted, which consists of a historical process which was based on the criticism of the aforementioned care. This movement, which began in 1980, had particularities according to the region of the country and was influenced by various currents, the historical context of the time and the successful replacement of the above model in other countries. In addition, it involved mobilizations in which health workers, people in psychological distress and their families wanted a more humane care(4-5).
These movements had a positive impact, culminating over the years in various measures, such as the sanction of Federal Law No. 10.216, which was fundamental for the consolidation of the federal government's mental health policy. This law affirms the rights and protection of people with mental disorders and redirects the mental health care model to a community care model (6) through the reduction of beds in psychiatric hospitals and the establishment of substitute services for previously existing hospital-centered psychiatric care, such as the Psychosocial Care Centers (CAPS), the Therapeutic Residential Services (TRS) and the Basic Health Units themselves (BHU)(4,6).
CAPS is a type of open, community and multidisciplinary health service that offers care to patients with persistent and severe MD and those with problems related to alcohol and other drug use in a given territorial unit(7). These institutions have as their main objective the reception of this public, their integration into social and family environments and the provision of support for the search for autonomy and medical and psychological care(8). These centers are organized into different types according to their complexity, the target audience and the number of inhabitants of the place. Thus, they are classified into CAPS I, II, III, Alcohol and Drugs (AD), AD III, Children (i)(7).
In these establishments, the work process takes place according to the severity of the users, with priority being given to the most serious disorders in this service. This assistance can be intensive, semi-intensive and non-intensive and requires daily, frequent and less frequent monitoring, respectively(9).
With an estimated population for 2018 of 117,014 individuals(10), Paulo Afonso/BA has, according to the National Register of Health Establishments(11), one CAPS II unit and one CAPS-ad unit, both of which are recommended to be installed in locations with a population of over 70,000(7). The site of this study was CAPS II by Paulo Afonso/BA, which was created in 2006 and provides care through a multidisciplinary team.
The objective of this study was, considering that there are no studies that address the characterization of the CAPS II of Paulo Afonso/BA, that the new model of mental health care is still in transition and that the knowledge of the clinical and sociodemographic aspects of public assisted in a particular health service is essential to guide the planning of strategies for its improvement, to analyze the characteristics related to age, gender, ethnicity, marital status, education level, occupation, city of residence, type of demand, type of treatment and diagnosis of users of the Psychosocial Care Center II of the city of Paulo Afonso - Bahia.
Method
A cross-sectional study was conducted at the Psychosocial Care Center II of the city of Paulo Afonso/BA, from April to June 2018.
During the study period, all active individuals (registered and attending the service) of all age groups, care regimens (non-intensive, semi-intensive or intensive) and cities of residence were included. attending CAPS II. Based on these criteria, 293 medical records were analyzed whose years of patient admission ranged from 2006 to 2018.
Data for analysis of clinical and sociodemographic profile was extracted from medical records, which refer to the current care modality, most recent psychiatric diagnosis, type of demand, age, sex, marital status, race /color, education level and occupation. The diagnostic hypotheses were presented in groups according to the tenth version of the International Classification of Diseases (ICD)(12). Simple frequencies and percentages of the study variables were calculated. Subsequently, Fisher's exact test was applied(13) to verify the association between gender and clinical diagnoses of users. The significance level adopted was less than 0.05 and the information obtained in the study was stored and analyzed using Microsoft Excel 2010 and Stata, version 12.0.
This work followed Resolution no. 466/2012 of the National Health Council and was approved with opinion number 2.547.699 by the Ethics and Research Committee of the Federal University of Vale do São Francisco (UNIVASF).
Results
The medical records of the 293 active users of CAPS II of the city of Paulo Afonso/BA were analyzed. The sample studied presented a higher proportion of individuals aged between 40 and 49 years (37.88%). Regarding gender, it was found that 163 patients were women (55.63%) and 130 men (44.37%). Regarding marital status, most individuals were single (165/56.31%) (Table 1).

Regarding occupation, the largest fraction of users was employed (104/35.49%). Regarding education, 121 (41.3%) did not have completed data regarding this variable. Among those who had information on this aspect, the majority (107/36.52%) had incomplete elementary school and illiteracy and the minority had incomplete and complete high school in equal proportion (2/0.68%) (Table 1).
Regarding the city of residence, only one of the users did not live in the city of Paulo Afonso/BA. Regarding the race/color variable, only nine records contained this data.
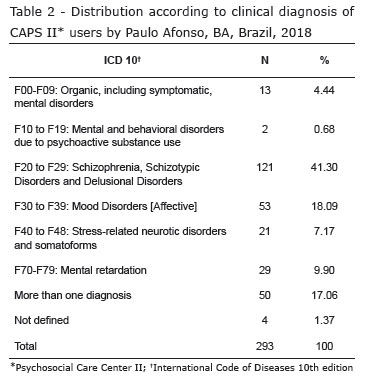
Of the clinical diagnoses, grouped into the International Classification of Diseases (ICD-10) categories, the most prevalent were schizophrenia, schizotypic and delusional disorders, with 121 subjects (41.3%), followed by mood disorders [affections], present in 53 patients (18.09%), and the combined diagnoses of 50 users (17.06%) (Table 2).
It was also observed that the predominant care regime corresponded to non-intensive care (210/71.67%), followed by semi-intensive care (60/20.48%) and intensive care (22/7.51%). Another finding was the admission of 165 patients (56.31%) in CAPS II through referrals and 128 users (43.69%) due to spontaneous demand.
Through an association between clinical diagnoses and the variable "gender", it was found that organic mental disorders (F00-F09), schizophrenia, schizotypic and delusional disorders (F20-F29) and mental retardation (F70-F79) predominated in males, while mood disorders (F30-F39) and stress-related and somatoform-related neurotic disorders (F40-F48) were more prevalent in females, with statistical significance (p = 0.00) (Table 3).
Discussion
The predominance of the adult and economically active population in this study is similar to what was found in other research on the epidemiology of mental disorders(14-18). Possible determinants of illness in this age group include poor housing, unemployment, separated/divorced/widowed marital status, and non-access to consumer goods(19). Although most of the medical records (51.88%) did not present information on occupation, the highest proportion (35.49%) was of the patients who were employed, which is a positive point, since working contributes to the self-worth of the individual by reaffirming his or her culturally depreciated capacity(20). In addition, a prospective study conducted in Vancouver, Canada showed that acquiring a job increased the psychological well-being of people with severe mental disorders(21).
Regarding the level of education detected, most were illiterate and had incomplete elementary school (107/36.52%). The predominance of low education in CAPS was also observed in other studies(16,22-24) and may be justified by the fact that most users of the Unified Health System have low education(25). Although in the process of improvement, there is still a considerable rate of people with poor education in Brazil, with the Northeast being the region with the highest illiteracy rate and the lowest average years of schooling(26). Other explanations would be that people with compromised mental health find it difficult to perform productive work and to exploit their potential(2). In addition, these individuals encounter barriers in educational institutions and are often excluded from the education process and, consequently, from the labor market(2).
Regarding marital status, most users (63.14%) were without a partner (single/divorced/widowed), and this finding is corroborated by other studies(15-16,22). Regarding the relationship mental health and love relationship, studies show that the impact of this type of relationship would depend on its nature, ie, if guided by maturity, dialogue, reciprocity, among other aspects, it would be beneficial to the individual with mental health, as it would stimulate their autonomy and personal growth. Otherwise, it would predispose to mental illness(27). On the other hand, marital status may be a consequence of the characteristics of certain mental disorders. Schizophrenia, for example, usually settles in patients between the ages of 10 and 25, and can lead to social withdrawal, apathy and loss of interest, all of which may make it difficult to build a more stable relationship. That way, most of these don't marry(28).
The predominance of females in the CAPS II of the city of Paulo Afonso is in line with other studies in this type of service(14-18) and may be related to the fact that men, in general, seek less health services due to cultural and institutional barriers(29). In addition, a systematic review on the prevalence of mental disorders in the Brazilian adult population showed that males are more affected by disorders related to psychoactive substance use, ie, it would be expected that there would be a predominance of men in the Psychosocial Care Centers for Alcohol and Drugs (CAPS-ad) of the study municipality, not CAPS II(19). Study conducted at CAPS - ad from Curitiba/PR obtained higher prevalence of males(30), what meets this hypothesis.
Regarding the prevalent disorders in women, studied found that females are more affected by mood disorders, anxiety and somatoforms(19), This corroborates the findings of this manuscript, since mood disorders (F30-F39) and stress-related and somatoform-related neurotic disorders (F40-F48) were also predominant in females (p = 0.00 ) at the CAPS II of Paulo Afonso/BA.
The most prevalent ICD category in this study, which was schizophrenia, schizotypic and delusional disorders (121/41.3%), also predominated in other surveys(17,22,31-32). Of the users with these disorders, 69 individuals (57.02%) were male, which goes against the epidemiology characteristic of schizophrenia, whose prevalence in both sexes is equivalent(33). However, this finding may be justified by the fact that schizophrenia, when in men, has earlier onset(28), present longer duration and be associated with a worse prognosis(1). Another aspect to be considered is that the higher prevalence of this ICD group in the study is consistent with the service provided by CAPS, which should provide care to the population with severe and persistent mental disorders(7). In primary care, by contrast, depressive and anxiety disorders are the most common(34).
Another clinical aspect observed was the predominance of the non-intensive treatment regimen (210/71.67%), which was also prevalent in a study conducted at the CAPS of Ilhéus/BA(31). The types of care depend on the individual's clinical condition, that is, they are defined based on an individualized analysis of each user's situation. Intensive care needs daily monitoring; semi-intensive, frequent and non-intensive, less frequent(9). In the CAPS II of the municipality under study, the intensive regime has daily follow-up, semi-intensive, twice a week and non-intensive, every 15 days or every ten days, depending on the case.
Regarding the form of entry into the CAPS under study, most were made through referrals (165/56.31%), a common practice in the Unified Health System (UHS), as its organizational principle is the hierarchy of services(35). However, some scholars argue that this model of referral and counter-referral system is related to a fragmentation of care, which tends to lead to a lack of accountability(36). For such a problem, an alternative would be the installation of a matrix service, which "consists of supervisory actions, shared care and in-service training, carried out by a mental health team for primary care teams or professionals"(37). This would be fundamental for the co-responsibility of care by the reference teams in mental health and primary care(37).
The lack of information in medical records, especially on occupation, education level and ethnicity, was a limiting point of the research. Another noteworthy limitation is that variables subject to change over time - education level, occupation and marital status - only appear once in the medical record, ie, reflect the individual's situation when he or she was admitted to the service, which does not necessarily match with the current reality.
Nevertheless, the study is extremely important for the characterization and analysis of CAPS II users from the city of Paulo Afonso/BA and for the foundation of therapeutic activities in the service, management discussions and awareness about the importance of knowing, registering and update the sociodemographic aspects of users. It is noteworthy that further studies in the CAPS of this city are essential since other aspects related to mental disorders can still be researched, such as triggering events, age of diagnosis, hospitalization rate and socioeconomic aspects.
Conclusion
The research allowed to characterize the users of CAPS II of the city of Paulo Afonso/BA, being found the highest prevalence of individuals with occupation, single, between 40 and 49 years old, with low education, admitted by referral, in non-intensive care and disorders of the group of schizophrenic, schizotypic and delusional disorders.
Considering that mental health services are in the process of improvement, it is expected that this work, pioneered in the CAPS II of Paulo Afonso/BA, will be used as a subsidy for the planning of interventions directed to certain groups and for development of improvement strategies, as well as fostering new research in this scenario.
Aknowledgements
We thank the staff of the Center for Psychosocial Care II of the city of Paulo Afonso/BA for their welcome during data collection and for the care provided to users of the service.
References
1. American Psychiatric Association. Manual diagnóstico e estatístico de transtornos mentais: DSM-5. 5. ed. Porto Alegre: Artmed; 2014. p. 20. [ Links ]
2. Chan M. Mental health and development: targeting people with mental health conditions as a vulnerable group. Geneva: World Health Organization; 2010. [ Links ]
3. World Health Organization. The World health report 2001: Mental health: new understanding, new hope. Geneva: World Health Organization; 2001. [ Links ]
4. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Caderno de atenção básica: Saúde Mental. Brasília, DF; 2013. [ Links ]
5. Oliveira AGB de, Alessi NP. Citizenship: instrument and finality of the working process in psychiatric reform. Ciênc Saúde Coletiva. [Internet]. 2005 Jan/Mar; 10(1):191-203. [cited Ago 4 2018]. Available from: <http://dx.doi.org/10.1590/S1413-81232005000100026> [ Links ].
6. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Coordenação Geral de Saúde Mental. Reforma psiquiátrica e política de saúde mental no Brasil. Conferência Regional de Reforma dos Serviços de Saúde Mental: 15 anos depois de Caracas. Brasília, DF; 2005. [ Links ]
7. Ministério da Saúde (BR). Portaria nº 3.088, de 23 de dezembro de 2011. Republicada em 21 de maio de 2013. Institui a Rede de Atenção Psicossocial para pessoas com sofrimento ou transtorno mental e com necessidades decorrentes do uso de crack, álcool e outras drogas, no âmbito do Sistema Único de Saúde (SUS). Brasília, DF. [Internet]. 2011. [Acesso 5 ago 2018] Disponível em: <http://bvsms.saude.gov.br/bvs/saudelegis/gm/2011/prt3088_23_12_2011_rep.html> [ Links ].
8. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Saúde mental no SUS: os centros de atenção psicossocial. Brasília, DF; 2004. [ Links ]
9. Ministério da Saúde (BR). Portaria nº 336, de 19 de fevereiro de 2002. Brasília, DF. [Internet]. 2011. [Acesso 3 ago 2018] Disponível em: <http://bvsms.saude.gov.br/bvs/saudelegis/gm/2002/prt0336_19_02_2002.html> [ Links ].
10. Instituto Brasileiro de Geografia e Estatística [homepage na internet]. Paulo Afonso. [Acesso 9 ago 2018]. Disponível em: <https://cidades.ibge.gov.br/brasil/ba/paulo-afonso/panorama> [ Links ].
11. Cadastro Nacional de Estabelecimentos de Saúde (CNES) [homepage na internet]. Estabelecimento de Saúde do Município: Paulo Afonso. [Acesso 9 ago 2018]. Disponível em: <http://cnes2.datasus.gov.br/Lista_Es_Municipio.asp?VEstado=29&VCodMunicipio=292400&NomeEstado=BAHIA> [ Links ].
12. Ministério da Saúde (BR). Departamento de Informática do SUS - DATASUS [homepage na internet]. Classificação Internacional de Doenças. Capítulo V - Transtornos mentais e comportamentais (F00-F99). [Acesso 9 jul 2018]. Disponível em: <http://www.datasus.gov.br/cid10/V2008/WebHelp/f00_f99.htm> [ Links ].
13. Altman DG. Practical statistics for medical research. Florida: CRC Press; 1990. [ Links ]
14. Oliveira VF de, Alves JS, Moraes ACS de, Silva JC, Silva CSS da, Nepomuceno FWAB, et al. Clinical characterization of patients with mental disorders assisted in psychosocial care center in São Francisco do Conde - Bahia. Rev Ciênc Méd Biol. [Internet]. 2014;13(2):204-11. [cited Jul 20 2018]. Available from: <http://dx.doi.org/10.9771/cmbio.v13i2.11672> [ Links ].
15. Soares AC, Trindade L, Rodrigues GCS, Silva FPA da, Sia EF. Clinical-epidemiological analysis of patients with mental disorders in the Brazilian Amazon. Rev Bras Neurol Psiquiatr. [Internet]. 2015;19(2):96-107. [cited Jul 15 2018]. Available from: <https://rbnp.emnuvens.com.br/rbnp/article/view/55> [ Links ].
16. Paula CTC. Profile epidemiological of the users of the Psychosocial Care Center in the city of Recife. Cad Bras Saúde Mental. [Internet]. 2010;2(4-5):94-106. [cited Jul 20 2018]. Available from: <http://incubadora.periodicos.ufsc.br/index.php/cbsm/article/view/1106> [ Links ].
17. Cruz, LS da, Carmo DC do, Sacramento DMS do, Almeida MSP de, Silveira HF da, Ribeiro HL Junior. Profile of patients with mental disorders assisted in the center for psychosocial care in the city of Candeias, Bahia, Brazil. Rev Bras Ciênc Saúde. [Internet]. 2016;20(2):93-8. [cited Ago 20 2018]. Available from: <https://doi.org/10.4034/RBCS.2016.20.02.01> [ Links ].
18. Bellettini F, Gomes KM. Profile of attendees of the psychosocial care center and mental health program in the city of Orleans-SC. Cad Bras Saúde Mental. [Internet]. 2013;5(12):161-175. [cited Ago 4 2018]. Available from: <http://incubadora.periodicos.ufsc.br/index.php/cbsm/article/view/1694/3192> [ Links ].
19. Santos EG dos, Siqueira MM de. Prevalence of mental disorders in the Brazilian adult population: a systematic review from 1997 to 2009. J Bras Psiquiatr. [Internet]. 2010;59(3):238-46. [cited Ago 4 2018]. Available from: <http://dx.doi.org/10.1590/S0047-20852010000300011> [ Links ].
20.Zambroni-de-Souza PC. Working with health: work and severe mental disorder. Psicol Estud. [Internet]. 2006;11(1):175-183. [cited Ago 12 2018]. Available from: <http://dx.doi.org/10.1590/S1413-73722006000100020> [ Links ].
21. Negrini A, Corbière M, Fortin G, Lecomte T. Psychosocial well-being construct in people with severe mental disorders enrolled in supported employment programs. Commun Ment Health J. [Internet]. 2014;50(8):932-42. [cited July 8 2019]. Available from: <https://doi.org/10.1007/s10597-014-9717-8> [ Links ].
22. Ballarin MLGS, Miranda IMS de, Carvalho CM de. Psychosocial Care Center in Campinas: a study on the socio-demographic and clinical profiles of its users. Rev Ciênc Méd. [Internet]. 2011;20(3-4):59-67. [cited Jun 12 2018]. Available from: <https://doi.org/10.24220/2318-0897v20n3/4a581> [ Links ].
23. Carvalho MDA de, Oliveira HS, Rodrigues LV. Epidemiological profile of users of the municipal Mental Health Care Network of Iguatu, Ceará, Brazil. SMAD Rev Eletron Saúde Mental Álcool e Drogas. [Internet]. 2010;6(2):337-49. [cited jun 22 2018]. Available from: <https://doi.org/10.11606/issn.1806-6976.v6i2p337-349> [ Links ].
24. Mangualde AAS, Botelho CC, Soares MR, Costa JF, Junqueira ACM, Vidal CEL. Epidemiological profile of patients treated in a Center for Psychosocial Care. Mental. [Internet]. 2013;10(19):235-48. [cited Jun 22 2018]. Available from: <http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1679-44272012000200006> [ Links ].
25. Silva ZP da, Ribeiro MCSA, Barata RB, Almeida MF de. Socio-demographic profile and utilization patterns of the public healthcare system (SUS), 2003- 2008. Ciênc Saúde Coletiva. [Internet]. 2011;16:3807-16. [cited Jun 15 2018]. Available from: <http://dx.doi.org/10.1590/S1413-81232011001000016> [ Links ].
26. Instituto Brasileiro de Geografia e Estatística. Pesquisa nacional por amostra de domicílios: síntese de indicadores 2015. Coordenação de Trabalho e Rendimento. Rio de Janeiro: IBGE; 2016. [ Links ]
27. Schlösser A. Interface between mental health and romantic relationship: a look from the positive psychology. Pensando Familias. [Internet]. 2014;18(2):17-33. [cited Jun 17 2018]. Available from: <http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1679-494X2014000200003> [ Links ].
28. Fontana AM. Esquizofrenia, Transtornos Esquizotípico e Delirantes. Manual de clínica em psiquiatria. São Paulo: Editora Atheneu; 2006. p. 277-294. [ Links ]
29. Gomes R, Nascimento EF do, Araújo FC de. Why do men use health services less than women? Explanations by men with low versus higher education. Cad Saúde Pública. [Internet]. 2007;23(3):565-74. [cited 12 Jun 2018]. Available from: <http://dx.doi.org/10.1590/S0102-311X2007000300015> [ Links ].
30. Ribeiro DR, Carvalho DS de. Drug use of groups in distinct phases of treatment in Psychosocial Care Centers for Alcohol and Drug (CAPS-AD). J Bras Psiquiatr. [Internet]. 2015;64(3):221-2. [cited Jun 12 2018]. Available from: <http://dx.doi.org/10.1590/0047-2085000000082> [ Links ].
31. Freitas AA, Souza RC de. Clinical and social demographic characterization of Psychosocial Care Centers (CAPS) users. Rev Baiana Saúde Pública. [Internet]. 2010;34(3):530-43. [cited Jun 29 2018]. Available from: <https://doi.org/10.22278/2318-2660.2010.v34.n3.a53> [ Links ].
32. Andreoli SB, Ronchetti SSB, Miranda AP de, Bezerra CRM, Magalhães CCPB, Martin D, et al. Utilization of community mental health services in the city of Santos, São Paulo, Brazil. Cad Saúde Pública. [Internet]. 2004;20(3):836-44. [cited Jun 23 2018]. Available from: <http://dx.doi.org/10.1590/S0102-311X2004000300021> [ Links ].
33. Sadock BJ, Sadock VA. Compêndio de psiquiatria: ciências do comportamento e psiquiatria clinica. 9. Ed. Porto Alegre: Artmed; 2007. [ Links ]
34. Souza LGS, Menandro MCS, Couto LLM, Schimith PB, Lima RP de. Mental Health in the Family Health Strategy: a review of Brazilian literature. Saúde Soc. [Internet]. 2012;21(4):1022-34. [cited Jun 22 2018]. Available from: <http://dx.doi.org/10.1590/S0104-12902012000400019> [ Links ].
35. Ministério da Saúde (BR). Secretaria Nacional de Assistência à Saúde. ABC do SUS: doutrinas e princípios. Brasília, DF; 1990. [ Links ]
36. Zambenedetti G, Perrone CM. Building a process of mental health care network: challenges and potentialities of the Psychiatric Reform. Physis. [Internet]. 2008;18(2):277-93. [cited Jun 17 2018]. Available from: <http://dx.doi.org/10.1590/S0103-73312008000200005> [ Links ].
37. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Saúde Mental no SUS: acesso ao tratamento e mudança do modelo de atenção. Relatório de Gestão 2003-2006.: Brasília, DF: Ministério da Saúde; 2007. [ Links ]
Received: Apr 9th 2019 Contribution of the authors: Study design and planning: Camila Gomes Barbosa, Paulo Roberto Marinho Meira, Joida Silva Nery. Data collection: Camila Gomes Barbosa, Bruno Bezerra Godim. Data analysis and interpretation: Camila Gomes Barbosa, Paulo Roberto Marinho Meira, Joida Silva Nery, Bruno Bezerra Godim. Manuscript writing: Camila Gomes Barbosa, Paulo Roberto Marinho Meira, Joida Silva Nery, Bruno Bezerra Godim. Critical review of the manuscript: Camila Gomes Barbosa, Paulo Roberto Marinho Meira, Joida Silva Nery, Bruno Bezerra Godim. Corresponding author:
Corresponding author:
Camila Gomes Barbosa
E-mail: camilagomesbarbosa95@gmail.com
Accepted: Ago 14th 2019
All authors approved the final version of the text.
Conflict of interest: the authors declare no conflict of interest.











 texto en
texto en 


