Servicios Personalizados
Articulo
Indicadores
Compartir
SMAD. Revista eletrônica saúde mental álcool e drogas
versión On-line ISSN 1806-6976
SMAD, Rev. Eletrônica Saúde Mental Álcool Drog. (Ed. port.) vol.16 no.2 Ribeirão Preto abr./jun. 2020
http://dx.doi.org/10.11606/issn.1806-6976.smad.2020.158506
ORIGINAL ARTICLE
Clinical characteristics of drug users hospitalized in an intensive care unit*
Gabriela Botelho PereiraI ; Karine Langmantel SilveiraI,II
; Karine Langmantel SilveiraI,II ; Carla Luciane dos Santos BorgesI
; Carla Luciane dos Santos BorgesI ; Michele Mandagará de OliveiraI
; Michele Mandagará de OliveiraI
IUniversidade Federal de Pelotas, Pelotas, RS, Brazil
IIBolsista da Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Brazil
ABSTRACT
OBJECTIVE: to describe causes of hospitalization and comorbidities of patients diagnosed with substance abuse / dependence admitted to an Intensive Care Unit.
METHOD: retrospective, descriptive-exploratory, cross-sectional and quantitative study.
RESULTS: a total of 865 medical records were analyzed between 2012 and 2015. The prevalence of substance use was 51.9%, of these 22% of total alcohol users and 48.7% tobacco. Among the users with diagnosed dependence, the main causes of hospitalization were Chronic Obstructive Pulmonary Disease (100%) and digestive hemorrhage (84%) and most patients presented more than one comorbidity simultaneously.
CONCLUSION: the results showed numerous causes of hospitalization and comorbidities that demonstrated the physical and mental impairment that may be related to excessive consumption of psychoactive substances.
Descriptors: Substance-Related Disorders; Drug Users; Intensive Care Unit; Comorbidities.
Introduction
The abuse of alcohol and other drugs represents a serious public health problem, as it can progress slowly and insidiously, progressing to chronification, causing serious problems in the health-disease process of the individual, family and society(1).
The impact of drug abuse on society as a whole is incalculable in all countries, as it relates to the possibility of comorbidities, early mortality, increased violence and crime, traffic and work accidents, absenteeism, emotional disturbances, family and social conflicts(2).
Consumption of alcohol, tobacco and other licit drugs is increasing and clearly contributing to the burden of disease worldwide. Most of the world's problems arising from psychoactive substance use come from licit drugs. Tobacco and alcohol appear to be major causes of mortality and disability in developed countries and important risk factors in terms of preventable disease burden in Latin America. Alcohol consumption is the third leading cause of disease and premature death worldwide, 3.3 million deaths and 5.1% of the global burden of disease(3-4).
Assistance to users of alcohol and other drugs should be provided at all levels of care, focusing on out-of-hospital devices, but in cases of clinical complications, hospital institutions are strategic locations in the health care network. When critically ill, this population may need access to hospitalization in Intensive Care Units (ICU).
Given the above and the scarcity of studies on the subject, this research aims to describe the causes of hospitalization, comorbidities and clinical characteristics of this population, when hospitalized in an Intensive Care Unit.
Method
Retrospective, descriptive, cross-sectional and quantitative study using a secondary data source, conducted at a teaching hospital in the city of Pelotas - Rio Grande do Sul, which exclusively serves users of the Unified Health System, specifically in the ICU. The ICU studied is composed of six beds, receiving clinical and surgical patients, excluding trauma hospitalizations, cardiac and neurological surgeries.
To calculate the sample, based on the literature, it was estimated that the prevalence of alcohol and other drug abuse in ICU patients is 25%, since it was the study that most closely resembled the investigated population and methodology. With a tolerable error of ± 3 percentage points and 95% confidence level, a sample size of 880 patients was calculated using the EPI INFO software(5).
In order to reach the estimated sample size, the number of hospitalizations retrospectively was verified by counting, using the unit's hospitalization register. Initially, it was estimated that to reach the sample size would require five years of survey and an average number of annual hospitalizations of 200 users, but the number was reached in four years of survey.
A table was prepared with the number of medical records of all patients admitted to the ICU, from 2012 to 2015, taken from the unit's hospitalization register. Subsequently, the data were searched in the Medical and Statistical Archive Sector (MSAS). A pre-elaborated instrument with closed and coded questions was applied.
The identification of medical records and data collection were performed by the author of the project. Thirty charts per collection shift were searched during three days of the week, covering 90 records per week, reaching the proposed sample in approximately ten weeks, during the months of July, August and September 2016.
The dependent variable corresponded to the "diagnosis of alcohol / drug abuse / dependence". The independent variables were gender, age, marital status, occupation, type of substance used, comorbidities, mechanical ventilation time, cause of hospitalization, length of ICU stay and outcome of hospitalization.
The collected data was entered into MS Access (Microsoft Office Access). Initially, exploratory analyzes were performed to characterize the study population and to meet the proposed objectives using descriptive measures (mean, mode, median) and dispersion (standard deviation).
The second phase was to verify associations between the diagnosis of alcohol / drug abuse / use (outcome) and independent variables by applying Pearson's chi-square test or Fisher's exact test (frequencies <5).
Subsequently, the magnitude of the associations was estimated. The prevalence of hospitalized patients diagnosed with abuse of alcohol and other drugs was used and, as a measure of association, the Prevalence Ratio (PR) and its respective 95% confidence intervals, estimated as a function of the relative incidence of Poisson's Regression method using the robust variance method. The statistical significance level of 5% (α < 0.05) was adopted.
The study observed the Code of Ethics of Nursing Professionals, based on Resolution COFEN 311/2007, Chapter III, Art. 89, 90 and 91, and Resolution No. 466/2012 of the National Health Council, being approved by the Research Ethics of the Faculty of Medicine of the Federal University of Pelotas under opinion No. 1.540.724.
Results
877 medical records of patients admitted to the Intensive Care Unit (ICU) were identified, during the period 2012-2015. Of the total, 12 medical records were excluded because they were not located in the archiving service and represented 1.7% of the total during the period with 865 records remaining (n = 865).
In the defined period, the prevalence of hospitalized patients diagnosed with alcohol and other drug abuse was 51.9% (n = 449). The average age of the patients diagnosed as dependent on alcohol and other drugs was 59.3 ± 15.31 years and the male gender was predominant (68.9%) among the dependent, while among the non-dependent, the female gender predominated (65.1%).
The prevalence of alcohol users in the ICU total population is 22%; tobacco, 48.7%; cannabis, 3%; cocaine, 2.3%; of crack, 2.7% and of other drugs, 0.1%, and 22% of the total inmates were multiple drug users. The average time of alcohol consumption was 26.3 ± 10.2 years; tobacco was 35.6 ± 13.2 years; marijuana was 15.4 ± 6.2 years; cocaine, 14.5 ± 6.9 years and crack, 9.6 ± 4.7 years.
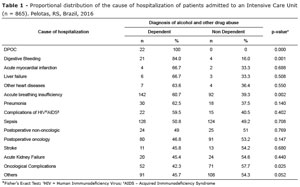
The table below shows the proportional distribution of the cause of hospitalization of patients admitted to the ICU.
Regarding the comorbidities of ICU patients, most patients presented more than one comorbidity simultaneously. Of those with cardiovascular comorbidities, users diagnosed with alcohol and other drug abuse were 47.4%; respiratory, 72.7%; infectious, 60.3%; neoplasms, 51.8%; neurological, 32.1%; renal or metabolic, 35.3%; gastrointestinal, 78.1% and psychiatric, 31.2%.
Major cardiovascular comorbidities include systemic arterial hypertension, acute myocardial infarction and arrhythmias. The main respiratory diseases were acute respiratory failure, COPD and acute pulmonary edema. Among the infectious ones, sepsis, pneumonia, AIDS and opportunistic infections. Among the neoplasms, the main were the digestive tract, hematologic and pulmonary. Of the neurological comorbidities, the main one was stroke. Among the renal or metabolic diseases, the main ones were Diabetes Mellitus, acute and chronic kidney failure and diabetic ketoacidosis. The main gastrointestinal disorders were upper gastrointestinal bleeding and liver cirrhosis, and the most common of the psychiatric comorbidities were depression, anxiety and bipolar affective disorder.
Table 2 evaluated the magnitude of associations between ICU admissions of dependent patients compared to non-dependent patients according to clinical characteristics.
Discussion
The abuse of psychoactive substances is related to damage to the mental and physical health of users and, among the main physical consequences are liver problems, problems related to withdrawal syndrome, sleep impairment and gastrointestinal disorders(2).
Regarding the causes of hospitalization, the study showed that 100% of COPD patients were diagnosed with drug abuse or dependence, which may be related to the high prevalence found in ICU tobacco users (48.7%). Tobacco-related diseases are a major cause of hospitalization, especially in the elderly, and reduced smoking contributes to decreased morbidity and mortality(6).
Tobacco, alcohol and illicit drugs are among the top 20 risk factors for disease. This is due to the global burden due to diseases associated with tobacco use (years of inability to adapt to life - DALY). Tobacco is estimated to account for 8.8% of all deaths and 4.1% of DALY(7).
Smoking currently accounts for 45% of all cancer deaths, 95% of lung cancer deaths, 75% of COPD deaths and 35% of cardiovascular disease deaths(6).
The study showed that 22% of patients diagnosed with abuse or dependence on alcohol and other drugs were multiple drug users. Psychiatric predictors that encourage cigarette smoking include abuse of alcohol and other psychoactive drugs, as well as attention deficit disorder and depressive symptoms(4).
It was found that 84% of hospitalizations for digestive hemorrhage and 66.7% of hospitalizations for liver failure were from patients diagnosed with abuse or dependence on alcohol and other drugs. An Irish study found that among 170 patients admitted to the ICU for liver disease, 62 were alcohol-dependent (36.5%). In the United Kingdom, liver disease is the third most common cause of premature death, and over one million hospitalizations per year are the result of alcohol-related disorders(7-8).
Excessive alcohol consumption, according to the literature, maintains a causal relationship with more than 200 types of diseases and injuries, and may be the main cause of hospitalization. Alcohol consumption increases the risk of development or is associated with the worsening of various conditions, such as cancer, hypertension, cerebrovascular disease, acute myocardial infarction, liver disease, tuberculosis, diabetes, liver cirrhosis, osteoporosis, HIV/AIDS, and psychiatric complications and cases of aggression with serious consequences(9).
Of the patients admitted to the ICU for complications related to HIV / AIDS, 59.5% had a diagnosis of alcohol and other drug abuse, a prevalence similar to that found in the literature in a Canadian study, which was 56%. The use of injecting drugs, such as cocaine and opioids, can provoke local or widespread infectious and inflammatory diseases, and is closely associated with the spread of human immunodeficiency viruses (HIV) and hepatitis through the sharing of syringes. In this research, the use of injectable heroin was not identified, however, there were several records of intravenous cocaine(10-11).
Of the hospitalizations for sepsis, 50.8% were diagnosed with abuse or dependence on alcohol and other drugs. The literature confirms the relationship between sepsis and alcohol dependence from a US study that researched 11651 ICU admission records over a five-year period and found a 12% prevalence of alcohol dependence, lower than this study. These patients had higher rates of sepsis (12.9% vs 7.6%, p<0.001), organ failure (67.3% vs 45.8%, p<0.001), septic shock (3.6% vs 2.1%, p = 0.01) and hospital mortality (9.4% vs 7.5%, p = 0.022) in unadjusted analyzes. After adjusting for factors with known association with sepsis, alcohol dependence remained associated with sepsis, septic shock and in-hospital mortality(11).
It is important to discuss the issue of the diagnosis of alcohol and other drug use, since the unit investigated does not use a validated diagnostic scale and the information is strongly linked to that reported by patients and family members. The strategy of assessing consumption only from the interviewee's report possibly results in the occurrence of information bias due to the omission of abusive consumption by the interviewees, which possibly results in an underestimation of the prevalence(4).
The presence of cardiovascular comorbidities is consistent with the results of other studies that associate psychoactive substance use and system alterations, such as alcohol with increased blood pressure, dysregulation of triglycerides and lipids, higher risk of acute myocardial infarction and other cardiovascular diseases. A study conducted in Brazil observed a 25% prevalence of hypertension among CAGE patients (acronym for their four questions - Cut down, Annoyed by criticism, Guilty and Eye-opener). Hypertension has multifactorial involvement, however, it is believed that excessive alcohol consumption is the second non-genetic risk factor for the disease(9-13).
Significant prevalence of gastrointestinal comorbidities (78.1%) was found among hospitalized patients diagnosed with alcohol abuse or dependence and other drugs probably related to alcohol abuse. A study of patients admitted to a clinical inpatient unit diagnosed with alcoholism found a prevalence of 77.8% of alcoholic hepatitis, 60% of liver cirrhosis and 26.7% of upper gastrointestinal bleeding. About 35% of cirrhotic patients with esophageal or gastric varices are believed to bleed in the future and more than 20% will die in the first episode(9).
Regarding psychiatric comorbidities, the study corroborates others that show that mood disorders such as depression, uni or bipolar, and anxiety disorders are prevalent among psychiatric comorbidities associated with chemical dependence, with less frequent pathologies with psychotic symptoms. A study conducted in therapeutic communities observed a high prevalence of psychiatric comorbidities (88.8%) and, specifically, major depressive disorder (36.7%) and antisocial personality disorder (76.7%)(12).
The severity of ICU patients diagnosed with abuse or dependence on alcohol and other drugs was found to be severe, since the likelihood of the outcome of hospitalization occurring is 1.2 times higher (95% CI: 1.0-1, 2); of prolonged hospitalizations lasting 15 to 20 days is 1.7 times higher (95% CI: 1.3-2.1) and 1.2 times higher than mechanical ventilation (95% CI: 1, 1-1,4), when compared to non-dependent.
The average time of ICU stay ranges from four to ten days, and the length of stay in the ICU is associated with poor prognosis in patient recovery as well as high economic costs. MV is a frequent treatment and provides numerous benefits for the treatment of critically ill patients. However, the longer the MV, the longer the hospital stay, increasing the risk of complications(14-15).
It is important to mention that this study demonstrates a face of the public health problem, which is the abuse of psychoactive drugs, which has direct or indirect connection with social determinants and, in this context, needs resolute public policies that can strengthen the social, economic and health conditions of users and the community(16).
The results and literature have shown numerous causes of hospitalization and clinical and psychiatric comorbidities that may be associated with excessive use of alcohol and other drugs in patients requiring intensive care.
Final considerations
This research showed the main causes of hospitalization, the most frequent comorbidities and clinical characteristics of intensive care unit patients diagnosed with abuse or dependence on alcohol and other drugs, showing physical and mental impairment that may be related to excessive psychoactive substance use.
It was evidenced that, due to several pathologies and their negative evolution, patients who use alcohol and other drugs may reach critical situations and need ICU admission.
The limitations of the study were related to medical records, due to lack of information on use patterns and diagnosis of substance use disorders, as there is no standardization of diagnostic scale. The research helped to know the issue of psychoactive substance abuse during ICU stay, the severity of the diseases that affect them, so that full care can be offered to users. Still came to fill a knowledge gap, because there is little production on the theme.
Knowing this reality, the health team can be prepared to attend not only to the cause of hospitalization and the main comorbidities, but also to value the use of psychoactive substances to better plan the therapy, provide guidance to patients and family members and properly refer the user within the health care network.
References
1. Nascimento LTR, Souza J, Gaino LV. Relacionamento entre familiar e usuário de álcool em tratamento em um centro de atenção psicossocial especializado. Texto Contexto Enferm. 2015;24(3):834-41. doi: http://dx.doi.org/10.1590/0104-07072015003610013 [ Links ]
2. Silva ER, Ferreira ACZ, Borba LO, Kalinke LP, Nimtz MA, Maftum MA. Impacto das drogas na saúde física e mental de dependentes químicos. Cienc Cuidado Saúde. 2016 Jan/Mar; 15(1):101-8. doi: http://dx.doi.org/10.4025/cienccuidsaude.v15i1.27137 [ Links ]
3. Barbosa MB, Pereira CV, Cruz DT, Leite ICG. Prevalência e fatores associados ao consumo de álcool e de tabaco em idosos não institucionalizados. Rev Bras Geriatr Gerontol. 2018;21(2):125-35. http://dx.doi.org/10.1590/1981-22562018021.170185 [ Links ]
4. Garcia LP, Freitas LRS. Consumo abusivo de álcool no Brasil: resultados da Pesquisa Nacional de Saúde 2013. Epidemiol Serv Saúde. 2015; 24(2):227-237. doi: http://dx.doi.org/10.5123/S1679-49742015000200005 [ Links ]
5. Geary T, O'Brien P, Ramsay S, Cook B. Scottish Intensive Care Trainees Audit Share Group. A national servisse evaluation of the impacto of alcohol on admissions to Scottish Intensive Care Units. Anaesthesia. 2012 Oct; 67 (10):1132-7. doi: https://doi.org/10.1111/j.1365-2044.2012.07233.x [ Links ]
6. Marques AP, Montilla DER, Almeida WS, Andrade CLT. Internação de idosos por condições sensíveis a atenção primária à saúde. Rev Saúde Pública. 2014;48(5):819-26. https://doi.org/10.1590/S0034-8910.2014048005133 [ Links ]
7. Fröhlich S, Murphy N, Kong T, Ffrench-O'Carroll R, Conlon N, Ryan D et al. Alcoholic liver Disease in the intensive care unit - outcomes and predictors of prognosis. J Crit Care. 2014;29(6):1137.e7-1131.e13. doi: https://doi.org/10.1016/j.jcrc.2014.06.002 [ Links ]
8. Williams R, Aspinall R, Bellis M, Camps-Walsh G, Cramp M, Dhawan A, et al. Addressing liver disease in the UK: a blueprint for attaining excellence in health care and reducing premature mortality from lifestyle issues of excess consumption of alcohol, obesity, and viral hepatites. Lancet. 2014;384:1953-97. https://doi.org/10.1016/S0140-6736(14)61838-9 [ Links ]
9. OPAS Brasil - Organização Pan-Americana da Saúde. Folha informativa - álcool. Brasília; 2019. [Acesso 5 jul 2019]. Disponível em: https://www.paho.org/bra/index.php?option=com_content&view=article&id=5649:folha-informativa-alcool&Itemid=1093 [ Links ]
10. Santos RB. Prevalência e fatores associados à infecção pelo hiv entre usuários de drogas lícitas e ilícitas. Dissertação [Mestrado Ciências da Saúde]. Recife: Universidade Federal de Pernambuco; 2014. URL: https://repositorio.ufpe.br/handle/123456789/17744 [ Links ]
11. O'Brien JM Jr, Lu B, Ali NA, Martin GS, Aberegg SK, Marsh CB et al. Alcohol dependence is independently associated with sepsis, septic shock and hospital mortality among adult intensive care unit patients. Crit Care Med. 2007;35(2):345-50. doi: https://doi.org/10.1097/01.CCM.0000254340.91644.B2 [ Links ]
12. Danieli RV, Ferreira MBM, Nogueira JM, Oliveira LNC, Cruz EMTN, Araújo Filho GM. Perfil sociodemográfico e comorbidades psiquiátricas em dependentes químicos acompanhados em comunidades terapêuticas. J Bras Psiquiatr. 2017;66(3):139-49. doi: 10.1590/0047-2085000000163 [ Links ]
13. Capistrano FC, Ferreira ACZ, Silva TL, Kalinke LP, Maftum MA. Perfil sociodemográfico e clínico de dependentes químicos em tratamento: análise de prontuários. Esc Anna Nery. 2013;17(2):234-41. doi: http://dx.doi.org/10.1590/S1414-81452013000200005 [ Links ]
14. Sousa MNA, Cavalcante AM, Sobreira REF, Bezerra ALD, Assis EV, Feitosa ANA. Epidemiologia das internações em unidade de terapia intensiva. C&D Rev Eletrôn Fainor. (Vitória da Conquista). 2014;7(2):178-86. Disponível em: http://srv02.fainor.com.br/revista/index.php/memorias/article/view/288 [ Links ]
15. Murakami FM, Yamaguti WP, Onoue MA, Mendes JM, Pedrosa RS, Maida ALV et al. Evolução funcional de pacientes graves submetidos a um protocolo de reabilitação precoce. Rev Bras Ter Intensiva. 2015;27(2):161-9. Disponível em: http://www.scielo.br/pdf/rbti/v27n2/0103-507X-rbti-27-02-0161.pdf [ Links ]
16. Ventura CAA. Determinantes Sociais de Saúde e o uso de drogas psicoativas. SMAD - Revista Eletrônica Saúde Mental Álcool e Drogas. 2014;10(3):110. doi: http://dx.doi.org/10.11606/issn.1806-6976.v10i3p110-110 [ Links ]
 Corresponding Author:
Corresponding Author:
Gabriela Botelho Pereira
E-mail: enfagabi@bol.com.br
Received: May 30th 2019
Accepted: July 26th 2019
Authors' Contributions: Study design and planning: Gabriela Botelho Pereira, Michele Mandagará de Oliveira. Data collection: Gabriela Botelho Pereira, Michele Mandagará de Oliveira. Data analysis and interpretation: Gabriela Botelho Pereira, Karine Langmantel Silveira, Carla Luciane dos Santos Borges, Michele Mandagará de Oliveira. Preparation and writing of the manuscript: Gabriela Botelho Pereira, Carla Luciane dos Santos Borges. Critical revision of the manuscript: Carla Luciane dos Santos Borges, Michele Mandagará de Oliveira.
All authors approved the final version of the manuscript.
Conflict of interest: the authors declare no conflict of interest.
* Paper extracted from master's thesis “Prevalência de abuso de álcool e outras drogas em pacientes internados em Unidade de Terapia Intensiva”, presented to Universidade Federal de Pelotas, Pelotas, RS, Brazil.











 texto en
texto en