Serviços Personalizados
artigo
Indicadores
Compartilhar
Estudos e Pesquisas em Psicologia
versão On-line ISSN 1808-4281
Estud. pesqui. psicol. vol.21 no.spe Rio de Janeiro 2021
http://dx.doi.org/10.12957/epp.2021.64035
Estudos e Pesquisas em Psicologia
2021, Vol. spe. doi:10.12957/epp.2021.64035
ISSN 1808-4281 (online version)
PSICOLOGIA SOCIAL
Psychological Suffering, Medicalization and Women: Contributions in the Field of Public Health
Luciana Fernandes de Medeiros*, I ; Gisely da Costa Araújo**, I
; Gisely da Costa Araújo**, I ; Loyanne Monyk Torres Costa***, I
; Loyanne Monyk Torres Costa***, I ; Isabelly Cristina Soares de Oliveira****, I
; Isabelly Cristina Soares de Oliveira****, I ; Renata Meira Veras*****, II
; Renata Meira Veras*****, II
I Universidade Federal do Rio Grande do Norte - UFRN, Santa Cruz, RN, Brasil
II Universidade Federal da Bahia - UFBA, Salvador, BA, Brasil
Endereço para correspondência
ABSTRACT
In recent years we have seen a growing psychological suffering in women attended in primary health care in developing countries. This paper aims to analyze psychological suffering in a small city in northeastern Brazil and its relationship with medicalization. We applied 202 SRQ-20 questionnaires in 3 Basic Health Units in the first research step, which were analyzed with statistical support. In the second step, four women were interviewed in the primary health care service and the data were analyzed from Institutional Ethnography perspective. The results demonstrated a high number of primary health care users in psychological suffering (47.02%). The data also points to a significant prevalence of women in psychological suffering, the use of medicines and the struggles in dealing with the difficulties of everyday life. The medicalization of psychological suffering appeared several times in this study through the invisibility of these sufferings under the blanket of biomedical and medicalizing discourse. Those facts can affect contemporary women and the contradictions of being a woman in a capitalist and patriarchal society.
Keywords: psychological suffering, medicalization, institutional ethnography.
Sofrimento Psicológico, Medicalização e Mulher: Contribuições no Campo da Saúde Pública
RESUMO
Nos últimos anos temos visto um crescimento de sofrimento psicológico em mulheres atendidas na assistência de saúde primária em países em desenvolvimento. Este artigo teve como objetivo analisar o sofrimento psicológico em uma pequena cidade no Nordeste do Brasil e sua relação com a medicalização. Aplicamos 202 questionários SRQ-20 na primeira etapa da pesquisa em 3 unidades de saúde pública. Na segunda etapa, quatro mulheres foram entrevistadas e os dados foram analisados com o apoio da Etnografia Institucional. Os resultados demonstraram um alto número de usuários dessas unidades de saúde pública em sofrimento psicológico (47,02%). Esses dados também apontaram para uma prevalência significante de mulheres em sofrimento psicológico, o uso de medicamentos e o esforço em lidar com as dificuldades cotidianas. A medicalização do sofrimento psicológico apareceu diversas vezes nos relatos analisados neste estudo, evidenciando a invisibilidade desses sofrimentos através do discurso biomédico e medicalizante. Esses fatores desvelam as dificuldades em viver na contradição de ser mulher na contemporaneidade inserida numa sociedade que se revela capitalista e patriarcal.
Palavras-chave: sofrimento psicológico, medicalização, etnografia institucional.
Angustia Psicológica, Medicalización y Mujeres: Contribuciones en el Campo de la Salud Pública
RESUMEN
En los últimos años, hemos visto un aumento de la angustia psicológica en las mujeres atendidas en la atención primaria de salud en los países en desarrollo. Este artículo tuvo como objetivo analizar el sufrimiento psicológico en un pequeño pueblo del noreste de Brasil y su relación con la medicalización. Aplicamos 202 cuestionarios SRQ-20 en la primera etapa de la investigación en 3 unidades de salud pública. En la segunda etapa, cuatro mujeres han sido entrevistadas y los datos fueron analizados con el apoyo de la Etnografía Institucional. Los resultados mostraron un alto número de usuarios de estas unidades de salud pública en problemas psicológicos (47.02%). Estos datos también apuntaron una prevalencia significativa en las mujeres con problemas psicológicos, el uso de medicamentos y el esfuerzo para hacer frente a las dificultades diarias. La medicalización del sufrimiento psicológico apareció varias veces en los informes analizados en este estudio, mostrando la invisibilidad de estos sufrimientos a través del discurso biomédico y medicalizante. Estos factores revelan las dificultades para vivir en la contradicción de ser mujer en los tiempos contemporáneos insertos en una sociedad que se revela capitalista y patriarcal.
Palabras clave: sufrimiento psicológico, medicalización, etnografía institucional.
In the literature about psychological suffering in public health, the term "common mental disorders" (CMD) is also known as minor psychiatric disorders which represents the least severe and most frequent mental disorders (Tofoli, 2006). According to several studies (Parreira et al., 2017; Portugal, Campos, Gonçalves, Mari, & Fortes, 2016; Pinho & Araújo, 2012; Goldberg & Huxley, 1992), CMD include non-psychotic depression, anxiety and somatoform symptoms, with common symptoms such as: insomnia, fatigue, forgetfulness, irritability, concentration difficulties, different somatic complaints and feelings of low self-esteem, uselessness, sadness.
The CMD can generate suffering and also can decrease the quality of life of the affected people. It also causes economic burden in society, mainly due to the indirect costs related to absenteeism due to disease (Portugal et al., 2016). In addition, depressive symptoms may act in comorbidity with other chronic diseases such as heart problems, diabetes and cancer (Soegaard, 2012).
The subject of psychological suffering has been studied by some researchers (Traverso-Yépez & Medeiros, 2005, Azevedo, 2014, Fernandes & Sanz, 2016), who have not found a match between the CMD and a corresponding organic etiology. However, in accordance with the contemporary perspective of the biomedical model to be legitimized as disease, most people with suffering symptoms seek health services looking for medications, mainly anxiolytics. Consequently, the health professionals themselves became unable to develop other health care practices, as long as patients just look for medications in the health services (Azevedo, 2014).
The movement for Health Reform and Psychiatric Reform in Brazil enabled a new conception of health and mental illness, expanding care in the face of psychological and psychiatric suffering. These changes allowed the creation of policies which aimed at inserting mental health care in primary care through the Basic Health Units (Ministério da Saúde, 2002). The need to implement more comprehensive care in primary care is a fact (Azevedo, Traverso-Yépez, 2010). However, it is necessary to direct research in order to understand how mental health care is being carried out in these places.
Thus, the present study aimed to analyze the level of psychological suffering in primary care users and how they deal with this situation.
Methodological Procedures
Field Research
This is a descriptive and exploratory research, with a quali-quantitative and cross-sectional approach, carried out with primary care users at 3 Basic Health Units in Santa Cruz, Rio Grande do Norte, Brazil. According to IBGE (2016), Santa Cruz has almost 40,000 inhabitants and the residents with relatively low income and low schooling predominate compared to other municipalities and other regions. The UFRN campus (Facisa) is located in Santa Cruz and the psychology and physiotherapy students who collaborate with this research study there. For a characterization of psychological suffering, the study was carried out in two steps: 1) application of Self Reporting Questionnaire (SRQ-20) and informal conversation about psychological suffering during its filling and 2) in-depth interviews with four participant women. The first step sought to identify the occurrence of psychological suffering in adults between 18 and 65 years, residents in Santa Cruz/RN/Brazil. This step was performed throughout the year of 2017 and we applied 202 questionnaires. Secondly, we developed the second step of this research when we aimed to analyze how people deal with psychological suffering by interviewing 4 women in this situation. It has been observed that the majority of people who answered the SRQ-20 were women. So, it was decided to interview them. These women were selected because they accepted the invitation after taking the test SRQ-20 to participate in this stage.
The SRQ-20 is a questionnaire for the identification of mental health problems in primary health care, validated in Brazil and recommended by the World Health Organization (WHO), especially in developing countries, because it meets the criteria in terms of ease of use and reduced cost. With sensivity ranging from 62.9 to 90% and specificity ranging from 44 to 95%, the choice of SQR-20 as a screening instrument came from the fact that this instrument has already been translated, tested and validated in Brazilian urban populations (Mari, 1987; Gonçalves, Stein, & Kapczinski, 2008). The SRQ-20 (version in which the 20 questions for screening for nonpsychotic disorders are used) has been used in several countries of different cultures for screening for nonpsychotic disorders (Harding et al., 1980; Reeler & Immerman, 1994). It brings 20 questions with answers "Yes" or "No", covering the different dimensions of psychological suffering. Four questions are about physical symptoms, and 16 are about psycho-emotional disorders. Initially, the cut-off score of the SRQ-20 for this study was set at 7/8, as performed by Mari (1987). The answers are based on the last 30 days and the final result varies from 0 to 20, since each "Yes" is assigned as a point (Fiorotti, Rossoni, Borges, & Miranda, 2010). If the participant reaches seven points or more, he/she probably is, at that time, in psychological suffering.
The questionnaire was applied by psychology and physiotherapy students who are properly trained. Respondents, before answering the 20 questions of the questionnaire, signed a Written Informed Consent Form (WICF) which reported the research objectives as well as the risks and benefits. Those interviewed also read and signed the WICF. The research was approved by the Research Ethics Committee of Facisa/UFRN under Protocol number 50118215.2.0000.5568.
The data were systematized in a Microsoft Excel spreadsheet according to absolute frequency (n) and percentage (%). After processing the data, a descriptive statistical analysis was performed.
As the SRQ-20 is an instrument for screening, not diagnosis, the determination of the cut-off point for case detection, with its sensitivity and specificity, needs to be done by comparison with the gold standard, i.e., standardized psychiatric interview (Gonçalves, Stein, & Kapczinski, 2008).
For this reason, it was considered important to analyze the informal conversations held during the application of the questionnaire. Thus, in the second stage of the research, the observations and interviews were analyzed based on the theoretical-methodological perspective of Institutional Ethnography.
Institutional Ethnography (IE) as a Way to Understand and Analyze Health Practices in Everyday Life
Institutional Ethnography (IE) is a theoretical-methodological perspective systematized by Canadian sociologist Dorothy Smith (2005) that has been used by some researchers in recent years to understand the actions developed in various institutions (Véras, 2011).
Smith (2005) began her journey with the goal of developing a sociology for women and, therefore, a sociology for people. In this sense, IE takes as theoretical and epistemological basis some currents of the social sciences such as symbolic interactionism and Ethnometodology, Marxist and Foucaultian thinking, as well as philosophical ideas based on phenomenology (Smith, 2005; Campbell & Gregor, 2002). With this set of assumptions, IE has a theoretical-epistemological basis that seeks to value and understand "the point of view of people effectively involved in the events in question, seeking to enable them to understand their everyday practices as part of broader social relations in which they are inserted" (Pinheiro, 2014, p. 17, translated by the authors).
The main concepts of IE are: texts, ruling relations and institutions. That is, it seeks to explain why people act in a certain way in a certain place (Fernandes & Sanz, 2016; Azevedo, 2014; Véras, 2011). The texts are the socially instituted documents and discourses that are part of the repertoire of actions, behaviors and attitudes of people in a certain institution. As an example, we can mention policies (health, social assistance, education), social contracts, the routine of the place, the flowchart, the hierarchy, among others. Thus, the texts organize "our discourses and practices, since they act as key in the conjuncture between the local settings of the daily lives of people and the normalized relations" (Véras, 2011, p. 60, translated by the authors).
Many texts go through everyday practices and some contribute to ruling relations. The ruling relations are inspired by the work of Michel Foucault and refer to relationships between people who live in a hierarchy of one over the other. These relationships are present in speeches and everyday practices so that some speeches overlap others and some practices are more considered or valued than others. In that way, in health institutions, for example, policies, power relations between health professionals, managers and users, as well as practices that are built into everyday life contribute to work processes and ways of acting in different health care services (Smith, 2005).
According to Smith (2005) and Véras (2011), IE aims to examine an institution as a whole, mapping and evaluating how social life is organized. It takes into account the power relationships and how the work process is activated. The analysis is always directed to new issues and perspectives that can always be object of reflection.
Thus, understanding how to organize the work processes in the day-to-day life of the institution is important to point out the limits and potentialities of those actions. In the case of Brazilian public health, it was observed that, in some contexts, the official documents are valued, but the daily practice differs a lot from what is stated in the texts because there are other underlying texts and also the ruling relations that permeate these actions (Azevedo, 2014; Smith, 2005).
About the analysis in IE, Azevedo (2014) asserts that the goalis not to reach absolute truths, but describe and explain existing social relations in that context from certain positions, including the researcher himself. In this way, knowledge is constructed from a particular look, with theoretical basis, as a possibility among many.
From these assumptions, the interviews of the four (04) women were analysed by reading and re-reading the transcripts, survey of topics and categories and, finally, the relationship of these topics with the existing literature on psychological suffering. One of the themes that most stood out in the process of analysis was the medicalization of suffering. For this reason, it was considered relevant to go deeper in the following discussion.
Results and Discussion
Psychological Suffering in a City of Northeast Brazil: Gender and Medicalization
In the study, 202 people answered the questionnaire SRQ-20 in the city of Santa Cruz/RN/Brazil. Of the respondents, 130 (64%) were women and 72 (36%) men. It was found that 47.02% of these people had a score greater than seven (07) that points out to a significant index of psychological suffering during the research process which corroborates with other studies conducted in different Brazilian territories using the SRQ-20 (Gonçalves, Stein, & Kapczinski, 2008; Moreira, Bandeira, Cardoso, & Scalon, 2011; Lucchese, Sousa, Bonfin, Veras, & Santana, 2014; Coutinho, Almeida Filho, & Mari, 1999). "During the application of the SRQ-20, many participants told their history full of psychological suffering. Deprivations and gender-based violence have been widely reported" (Field Journal).
The results also pointed that, among 130 respondent women, 54.61% (71) had a score greater than seven. Among 72 respondent man, this rate was 33.33% (24). These results corroborate with other studies that point out the high rate of Brazilian women in suffering (Costa, Dimenstein, & Leite, 2014; Costa & Ludermir, 2005). In Recife, a population study found a total prevalence of common mental disorders in primary health care of approximately 35% (Ludermir & Melo Filho, 2002). In Pelotas, the prevalence of minor psychiatric disorders in primary health care was 22,7%, with 17.9% among men and 26% among women (Lima, Soares, & Mari, 1999).
The SRQ-20 questionnaire has 20 questions about everyday life. As can be seen in Figure 1, it was observed that 70,8% of respondents have affirmed that they use to feel nervous, tense or worried; 48% sleep badly and feel unhappy and 46% are easily tired and easily frightened. This set of symptoms is also more prevalent in other studies (Araújo, Almeida, Santana, Araújo, & Pinho, 2006; Lucchese et al., 2014).
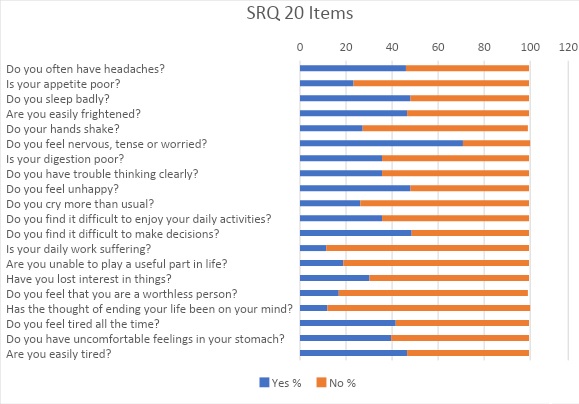
Figure 1. SQR 20 Results
There was also a higher rate of no responses to symptoms like daily work suffering. Although participants have demonstrated mainly symptoms as headaches, feeling nervous, being tired or finding it difficult to make decisions, the occupational activity was not considered a factor for the decrease in vital energy. Many of these symptoms characterize the so-called CMD (Parreira et al, 2017; Portugal, Campos, Gonçalves, Mari, & Fortes, 2016; Pinho & Araújo, 2012).
To better understand the life conditions of the participants, their observations were conducted and registered by field diaries and in-depth interviews. "In general, it was observed that many people come to health services with complaints of insomnia and/or anxiety asking the health care professional for a sleeping medication" (Field Diaries). It was also highlighted the use of psychotropic drugs by many participants. As the application was held in Basic Health Units, many people took the opportunity to talk with the researchers about their health condition. In this way, many participants complained about psychological symptoms and reported life experiences full of negative situations. "However, I have noticed that they had access only to the general practitioner and not to other health care practices." (Field Diaries).
Besides the participant observations, it was conducted in-depth interviews with 4 women which have scored more than 7 items in the SRQ-20 questionnaire. It was noticed that the interviewees tended to comment about their suffering intertwining it with situations experienced and present in daily life:
There were several changes in my brain, and I have strong emotions, anger, I suffer from attacks and I faint. So it's not good that I stay in the hall where there are people. I don't like it... Because I can fall anywhere, I have fallen and got injured, and my clothes shifted, revealing my body. I said I wanted that corner because I feel more protected. (Barbara, 49 years old)
There's no way of not feeling stressed. The routine is full of it, the coexistence of two is very difficult too, the family. I deal with people who make me feel angry every day. I had thyroid problems too. After this surgery, I was very nervous. (Carla, 47 years old)
The speeches of Barbara and Carla (fictitious names) denote the experience of a daily existence that brings ill-being and suffering under various orders. Emotions, common situations in everyday life and relationships are aspects that make these women get sick. Simões-Barbosa and Dantas-Berger (2017) have demonstrated that in the (contradictory) processes of socialization, women are educated to be emotional, dedicate themselves to the care of others and to not be competitive. These characteristics are contradictory to capitalist ideology, based on individualism and competition that requires objective, rational, aggressive and competitive behaviors. Thus, the daily sufferings of women can be the result of this contradiction, a constant struggle between the ideals of being a passive and emotional woman and the capitalist society. These ideals attributed to femininity are still very strong in Brazil, especially in the Northeast (Azevedo & Dutra, 2019). The participants tend to follow these ideals, but they tend not to reflect on it because it is part of an entire social imaginary.
It is evident, in these three moments of research, that everyday health practices seem to include the request of health care users who wish to get rid of uncomfortable symptom(s) and the need for health professionals to address health problems.
What is implicit in this relationship is that ruling relations can happen in two moments: when the professional, supposedly the one who has the knowledge, has the power to prescribe a "blue recipe" (popular term for psychotropic recipe), and when the non-specialist user, but with the power to make a scandal in the service when he/she cannot get the medicine, requires this medication or seeks another professional to satisfy it.
Parallel to this "demand" of users for medicines, most health workers does not know enough about psychological distress, and do not feel competent enough in this area to provide other care practices (Silveira, Almeida, & Carrilho, 2019). Thus, Bezerra, Morais, Paula, Silva and Jorge (2016) state that the exacerbated consumption of medicines is related to the hegemonic context and to the marketing social production of health, involving different actors, including: doctors, patients, pharmaceutical industry and health regulatory agencies. Therefore, drugs become socially valued and other health care practices remain invisible.
Consequently, what predominates in this context is the prescription of psychotropics due to complaints and symptoms of psychological suffering because, in this perspective, the user's demand goes through the same way as the health worker's: both will get rid of the problem in the way they were induced (by the pharmaceutical industry, for example), or by how they have learned (the hegemony of the biomedical model in health education, for example).
Silveira, Almeida and Carrilho (2019) also commented that
this is revealed in the speeches that brings out the insistence of the patients to request the prescription, the threats and aggressions that victimize the professionals and the complaints about the trafficking scheme to access controlled medicines. This is where we close the cycle into which benzodiazepines initially entered: its prescription is justified by the malaise caused by social conditions (drug trafficking and crime) and ends up sustaining the same trafficking and crime (pp. 118, translated by the authors).
Here, benzodiazepines are part of a context in which drug trafficking contributes to the suffering of people who, in their turn, get drugs from this same drug traffic to alleviate malaise.
When seeking health services, many users have nonspecific somatic complaints, which can lead to difficulties in the correct management of these manifestations of suffering. Thus, there is an underdiagnosis and abuse of benzodiazepines and unnecessary examinations and referrals commonly performed by health professionals (Silveira, Almeida, & Carrilho, 2019; Sousa, Maciel, & Medeiros, 2018). This practice is considered as medicalization of suffering, that is, any emotional, social or cultural aspect of daily life is now understood as a health problem and must be solved with medical technology. In the words of Bezerra et al. (2016), medicalization "refers to the incorporation of social, economic and existential aspects of human condition, such as sleep, sex, food and emotions, under the domain of the medicalizable, such as diagnosis, therapy, cure, etc." (p. 149, translated by the authors).
Even though the "demand" for the medication did not appear in the speeches of the interviewees, it is evident in the interview of the participant how the medication is valued:
... I am stressed, I think it's because of college things, homesickness, this sore throat, I am taking a medicine that is really bad, and stomachache. I've been to the nutritionist and she said that maybe it has to do with my diet, (...). For headache, I only take small doses of a medicine I have at home. (Carla, 19 years old)
The participant discourse highlighted the increasingly aggressive and naturalized medicalization of existential suffering. It is one of the most striking symptoms of this contemporary mode of health and experience of illness (Santos & Sá, 2013). According to Simões-Barbosa and Dantas-Berger (2017):
the medicalization of malaise resulting from various types of gender-based discrimination and violence that many women experience or witness – structural, institutional, ethnic-racial, urban violence, domestic, sexual, at work – has become a legitimate resource, generating what can be considered a pharmacological violence. (p. 4, emphasis added, translated by the authors)
And this pharmacological violence is made invisible by the postmodern ideals that emphasize speed, productivity and being always ready to respond to professional, social and affective demands. In the case of women, this is even more evident since social demands accentuate the feelings of unhappiness, inadequacy and frustration associated with psychic disorders (Simões-Barbosa & Dantas-Berger, 2017).
What is heard in services on a daily basis is that health workers are generally not satisfied with working conditions and resent the demands of users, who often want only the renewal of the prescription and nothing more. In a study on benzodiazepines in another northeastern city, the authors also found this difficulty among health professionals and users (Silveira, Almeida & Carrilho, 2019).
In the excerpt below, the participant says:
I had a long-term treatment with Dr. X and then I improved ... I took strong medicine for 5 years. I was "weaned" and I only took it at night. The symptoms disappeared with treatment. ... Then came the loss of my mother, she died of a heart attack ... At first, I acted normally, but when I realized it was real, the problems returned with the crises. I fell into depression. (Josefa, 51 years old)
In this discourse of Josefa, it can be observed how situations of loss contributed to her psychological suffering. However, when she really feels the loss of her mother, instead of grief, a process that is part of life, she gets sick and demands medication. In this sense, there is a very direct relationship between the suffering of life with illness and the consequent use of medicines.
Like Josefa, Silveira, Almeida & Carrilho (2019) have observed that many women enter health services with widespread complaints in order to be more likely to enter the benzodiazepine cycle of dependence, as they function in a rapid medical response, alleviating these inconvenient pains. It is the so-called chemical gag (Simões-Barbosa & Dantas-Berger, 2017). Socially and politically, women are required to assume various roles, but at the same time surreptitiously charged with maintaining a passive stance and adapting to the status quo: "Historically, disciplining the female body has been a surprisingly durable and flexible strategy for social control, with the health system being an important ally in the exercise of these (bio) power practices" (Simões-Barbosa & Dantas-Berger, 2017, p. 6, translated by the authors).
The participant continues talking about her complaints:
Yes, morning and night. I use carbamazepine and carbolytic because of the discovery of bipolar disorder. Sometimes, I have a sudden behavior change. ... but besides that, I fight a lot for myself, sometimes I avoid talking because I'm bipolar. I'm afraid that people willl misinterpret when I talk. Therefore, I avoid ... I fight for myself! ... Imagine, you are a good worker but you lose your job in an hour, I cried a lot. (Josefa, 51 years old)
Bezerra et al. (2016) comment that "the holder of the decision must be, in fact, the user, who, for that, must be informed about the risks and benefits of using the drug" (p. 152, emphasis added, translated by the authors), which is not what you see in Josefa's speech. There is some passivity in her speech when she says she is taking medication for a diagnosis of bipolar disorder. Have the risks and benefits of these medicines been discussed with her? Have other health care alternatives been considered? How long would she take these medications for?
Another worrying aspect is how Josefa deals with her diagnosis. She stops talking and expressing herself to others because she is "bipolar". Josefa is not a person anymore. She becomes her disease, attributed to her by some criteria (because, in other contexts, her symptoms would not have this connotation). This also characterizes the medicalization of life and suffering. Her ability to fight and to assume the political confrontation of the real causes of suffering is depotentiated, in addition to maintaining a licit drug market that sustains a business branch that has not shown any commitment to human wellness (Simões-Barbosa & Dantas-Berger, 2017).
Some texts on mental health care defend the psychosocial paradigm, which values one's autonomy, that is essential for mental health care. According to Sousa, Maciel and Medeiros (2018), the psychosocial paradigm is the result of Psychiatric Reform, which defends, among other principles, the right of the person to live in a free and autonomous way, with the support of family and interprofessional care. However, in the reality of services, what is seen is the presence of contradictions between the different texts (such as health policies X the biomedical paradigm) and the predominance of medicalizing practices. According to Bezerra et al. (2016), there is still a view anchored in the biomedical paradigm in relation to psychic suffering and mental health issues. In the conception of care in which there is a predominance of the clinical model, centered on the physician, people do not have the power to decide on their treatment, which implies lack of autonomy. The participant Josefa would be able to exercise her autonomy, since she says she is fighting for herself. But is this being valued in her daily life?
In this sense, medicalizing practices that strengthen the exclusion of the person are very evident in the context of this research. Even though health policies advocate welcoming and bonding with users of primary health care, this discourse is still very fragile in practice. Suffering is still considered eminently of biological/organic etiology and the search for the elimination of symptoms is the main goal of users as well as health professionals.
Final considerations
The results of this research demonstrated that there is a high number of people who have attended primary health care with psychological suffering. Most of them are women. Participant observations are fundamental in qualitative research, as long as the researcher can access the health care service, know its routine and establish relationships with workers and users, listening and participating in the actions developed. These are some of the main guidelines of IE, which is to know the service in depth, talk to people in their own workplace and know the resolutions, principles and protocols that govern the daily life of that institution. From this experience in the service, and with an attitude of openness to what comes, without so much prejudice and a priori ideas, it is possible to identify the limitations and possibilities of the context analyzed.
The researcher starts from a certain theoretical ballast to analyze a given phenomenon. An example of this is the psychological suffering itself that appears invisible to certain professional categories. Because it is not the focus of their work, and not having studied that theme, the health professional does not always give importance to the user's psychic complaints. It is very common for professionals to state that the problem of this or that patient is "only psychological" and "a relaxation would go well". With this discourse permeating their practice, the professional will probably not try to go into the users' history, nor understand their difficulties. Not because he is incompetent and inhuman, but because his understanding of psychic suffering is not part of his discourse and care practices. Psychic suffering and all its meanings and dimensions are not part of his texts.
No wonder they "created" a term to combine all diffuse symptoms so that they can standardize the diagnosis and treatment of these symptoms as the concept of common mental disorders (CMD). This concept is insufficient and its indiscriminate use can contribute to the medicalization of suffering and malaise because it categorizes in a vague diagnosis the experiences of being a woman in a still misogynistic and patriarchal context.
Thus, this professional is criticized by humanized professionals for not considering the social, economic, as well as gender issues, among others, which are related to psychological distress. Health professionals very rarely have this kind of discussion in their background.
There is a lot of difficulty in health services that aim to promote health, prevent disease and even cure the problems of the population when the team is made up of health professionals who, most of them, had technical and biological formation, especially since it is part of most pedagogical projects the in-depth study of the human body and the scientifically proven techniques of diagnosis, treatment, rehabilitation and cure.
A possible solution would be the inclusion of humanized professionals in health services. This has been done in some contexts such as the creation and development of multi-professional residences in university hospitals, for example. But there are other challenges: how to articulate the practices of these professionals with the daily life of a hospital? There are reports of health professionals who feel threatened by the presence of psychologists who will observe and criticize their practices. There are also psychologists who believe everything to be a dehumanizing process and who eventually assume the role of overseer of other professionals.
The capitalist logic also contributes to the use and abuse of medicines, strongly propagated by the pharmaceutical industry, as it promises immediate relief from troublesome symptoms. Moreover, this logic also permeates the consultation with the doctor who needs to be quick and efficient. This generates a contradiction between the capitalist logic (less time – more effectiveness) and the principles of primary health care that require welcoming and bonding (more time – greater depth). The problem is that by momentarily "relieving" what is bothering you could mean taking the risk of losing your psychic abilities and resources (or even learning them) to cope with life's difficulties.
Making chorus with so many other works on the subject, it is urgent to strengthen these discussions in health contexts and the search for less medicalizing care practices, aimed at health, well-being and happiness; practices that make social problems affecting part of the population visible and that provide alternative ways to lead life.
We understand that the limitations of the study are the lack of longitudinal monitoring of patients treated at the Basic Health Units. A longitudinal study could expand the daily challenges faced by users of the service.
References
Araújo, T. M., Almeida, M. M., Santana, C. C., Araújo, E. M., & Pinho, P. S. (2006). Psychological disorders among women: A comparative study between housewives and workers. Revista Enfermagem UERJ, 14(2), 260-9. Recuperado de https://www.researchgate.net/publication/317456529 [ Links ]
Azevedo, A. K. S., & Dutra, E. M. S. (2019). Era uma vez uma história sem história: Pensando o ser mulher no Nordeste. Pesquisas e Práticas Psicossociais, 14(2), 1-14. Recuperado de http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1809-89082019000200011&lng=pt&tlng=pt [ Links ]
Azevedo, L. F. M., & Traverso-Yépez, M. (2010). ‘De mãos atadas': O cotodiano dos trabalhadores a atenção básica em saúde diante do sofrimento psicológico. Saúde em Debate, 34(87), 726-733. Recuperado de https://www.redalyc.org/articulo.oa?id=406341768014
Azevedo, L. F. M. (2014). Os trabalhadores de Saúde Diante do Nervosismo: Uma Perspectiva a Partir da Etnografia Institucional. Saúde & Transformação Social, 5(1), 42-49. Recuperado de http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S2178-70852014000100008 [ Links ]
Bezerra, I. C., Morais, J. B., Paula, M. L., Silva, T. M. R., & Jorge, M. S. B. (2016). Uso de psicofármacos na atenção psicossocial: Uma análise à luz da gestão do cuidado. Saúde Debate, 40(110), 148-161. doi: 10.1590/0103-1104201611011 [ Links ]
Campbell, M., & Gregor, F. (2002) Mapping social relations: A primer in doing institucional etnography. Ontário: Garamond Press. [ Links ]
Costa, A. G., & Ludermir, A. B. (2005). Transtornos mentais comuns e apoio social: Estudo em comunidade rural da Zona da Mata de Pernambuco, Brasil. Cadernos de Saúde Pública, 21(1), 73-79. doi: 10.1590/S0102-311X2005000100009 [ Links ]
Costa, M. G. S. G., Dimenstein, M. D., & Leite, J. F. (2014). Condições de vida, gênero e saúde mental entre trabalhadoras rurais assentadas. Estudos de Psicologia, 19(2), 89-156. doi: 10.1590/S1413-294X2014000200007 [ Links ]
Coutinho, E. S. F., Almeida Filho, N., & Mari, J. J. (1999). Fatores de risco para morbidade psiquiátrica menor: Resultados de um estudo transversal em três áreas urbanas no Brasil. Revista de Psiquiatria Clínínica, 26(5), 246-256. Recuperado de http://www.hcnet.usp.br/ipq/revista [ Links ]
Fernandes, L., & Sanz, P. E. (2016). Los trastornos mentales comunes y la medicalización: Una perspectiva a partir de la etnografía institucional. Revista San Gregorio, 12, 7-15. Recuperado de https://revista.sangregorio.edu.ec/index.php/REVISTASANGREGORIO/article/view/147/1.pdf [ Links ]
Fiorotti, K. P., Rossoni, R. R., Borges, L. H., & Miranda, A. E. (2010). Transtornos mentais comuns entre os estudantes do curso de medicina: Prevalência e fatores associados. Jornal Brasileiro de Psiquiatria, 59(1), 17-23. doi: 10.1590/S0047-20852010000100003 [ Links ]
Goldberg D., & Huxley P. (1992). Common mental disorders: A bio-social model. London: Routledge. [ Links ]
Gonçalves, D. M., Stein A. T., & Kapczinski, F. (2008). Performance of the Self-Reporting Questionnaire as a psychiatric screening questionnaire: A comparative study with Structured Clinical Interview for DSM-IV-TR. Cadernos de Saúde Pública, 24(2), 380-90. doi: 10.1590/S0102-311X2008000200017 [ Links ]
Harding, T. W., De Arango, M. V., Baltazar, J., Climent, C. E., Ibrahim H. H. A., Ladrido-Ignacio, L., Murthy, R. S., & Wig, N. N. (1980). Mental disorders in primary health care: a study of their frequency and diagnosis in four developing countries. Psychological Medicine, 10(2), 231-41. doi: 10.1017/s0033291700043993 [ Links ]
Instituto Brasileiro de Geografia e Estatística. (2016). Censo Demográfico. Brasília, DF: IBGE. Recuperado de https://cidades.ibge.gov.br/brasil/rn/santa-cruz/panorama [ Links ]
Lima, M. S., Soares, B. G. O. & Mari, J. J. (1999). Saúde e doença mental em Pelotas, RS: Dados de um estudo populacional. Revista de Psiquiatria Clínica, 26(5), 225-35. Recuperado de https://pesquisa.bvsalud.org/portal/resource/pt/lil-256438 [ Links ]
Lucchese, R., Sousa, K., Bonfin, S. P., Veras, I. & Santana, F. R. (2014). Prevalência de transtorno mental comum na atenção primária. Acta Paulista de Enfermagem, 27(3), 200-207. doi: 10.1590/1982-0194201400035 [ Links ]
Ludermir, A. B., & Melo Filho, D. A. (2002). Condições de vida e estrutura ocupacional associadas a transtornos mentais comuns. Revista Saúde Pública, 36(2), 213-21. doi: 10.1590/S0034-89102002000200014 [ Links ]
Mari, J. J. (1987). Psychiatric morbidity in three primary medical care clinics in the city of São Paulo: Issues on the mental health of the urban poor. Social Psychiatry, 22(3), 129-38. doi: 10.1007/BF00583847 [ Links ]
Ministério da Saúde. (2002). Relatório Final da III Conferência Nacional de Saúde Mental. Brasília, DF: Conselho Nacional de Saúde. Recuperado de http://conselho.saude.gov.br/biblioteca/Relatorios/saude_mental.pdf [ Links ]
Moreira, J. K., Bandeira, M., Cardoso, C. S., & Scalon, J. D. (2011). Prevalence of common mental disorders in the population attended by the Family Health Program. Jornal Brasileiro de Psiquiatria, 60(3), 221-6. doi: 10.1590/S0047-20852011000300012 [ Links ]
Parreira, B. D. M., Goulart, B. F, Haas, V. J., Silva, S. R, Monteiro, J. C. S., & Gomes-Sponholz, F. A. (2017). Common mental disorders and associated factors: A study of women from a rural area. Revista da Escola de Enfermagem da USP, 51, 1-8. doi: 10.1590/s1980-220x2016033103225 [ Links ]
Pinho, P. S., & Araújo, T. M. (2012). Associação entre sobrecarga doméstica e transtornos mentais comuns em mulheres. Revista Brasileira de Epidemiologia, 15(3), 560-72. doi: 10.1590/S1415-790X2012000300010 [ Links ]
Pinheiro, V. S. (2014). A etnografia institucional: Notas teóricas introdutórias. In R. M. Veras (org.), Introdução à etnografia institucional: Mapeando as práticas na assistência à saúde (pp. 58-66). Salvador: EDUFBA. [ Links ]
Portugal, F. B., Campos, M. R., Gonçalves, D. A., Mari, J. J., & Fortes, S. L. C. L. (2016). Qualidade de vida em pacientes da atenção primária do Rio de Janeiro e São Paulo, Brasil: Associações com eventos de vida produtores de estresse e saúde mental. Ciência & Saúde Coletiva, 21(2), 497-508. doi: 10.1590/1413-81232015212.20032015 [ Links ]
Reeler, A. P., & Immerman, R. (1994). A preliminary investigation into psychological disorders among Mozambican refugees: Prevalence and clinical features. Central African Journal of Medicine, 40(11), 309-315. [ Links ]
Santos, D. G., & Sá, R. N. (2013). A existência como "cuidado": Elaborações fenomenológicas sobre a psicoterapia na contemporaneidade. Revista da Abordagem Gestáltica, 19(1), 53-59. doi: 10.1590/s0104-12902019180615 [ Links ]
Silveira, L. C., Almeida, A. N., & Carrilho, C. (2019). Os benzodiazepínicos na ordem dos discursos: De objeto da ciência a objeto gadget do capitalismo. Saúde e Sociedade, 28(1), 107-120. doi: 10.1590/S0104-12902019180615 [ Links ]
Simões-Barbosa, R. H., & Dantas-Berger, S. M. (2017). Abuso de drogas e transtornos alimentares entre mulheres: Sintomas de um mal-estar de gênero? Cadernos de Saúde Pública, 33(1), 1-11. doi: 10.1590/0102-311x00120816 [ Links ]
Smith, D. (2005) Institutional ethnography: A sociology for people. New York: Altamira Press. [ Links ]
Soegaard, H. J. (2012). Undetected Common Mental Disorders in Long-Term Sickness Absence. International Journal of Family Medicine, 2012, 1-10. doi: 10.1155/2012/474989 [ Links ]
Sousa, P. F., Maciel, S. C., & Medeiros, K. T. (2018). Paradigma Biomédico X Psicossocial: Onde são ancoradas as Representações Sociais acerca do sofrimento psíquico? Trends in Psychology, 26(2), 883-895. doi: 10.9788/tp2018.2-13pt [ Links ]
Tófoli, L. F. F. (2006). Transtornos somatoformes, síndromes funcionais e sintomas físicos sem explicação. In A. C. Lopes (Org.), Tratado de clínica médica (pp. 2507). São Paulo: Roca. [ Links ]
Traverso-Yepez, M., Medeiros, L. (2005). The Complexity of Symptoms and Meanings Involving "Nerves" in the Brazilian Public Health System. Qualitative health research, 15(9), 1231-1243. doi: 10.1177/1049732305277858 [ Links ]
Véras, R. M. (2011). Etnografia institucional: Conceito, usos e potencialidades em pesquisas no campo da Saúde. Saude & Transformação Social, 2(1), 58-66. Recuperado de http://incubadora.periodicos.ufsc.br/index.php/saudeetransformacao/article/view/560 [ Links ]
Endereço para correspondência
Luciana Fernandes de Medeiros
Facisa/UFRN, Santa Cruz - RN, Brasil. CEP 59200-000
Endereço eletrônico: lucianamedeirosufrn@gmail.com
Gisely da Costa Araújo
Facisa/UFRN, Santa Cruz - RN, Brasil. CEP 59200-000
Endereço eletrônico: giselyaraujo84@gmail.com
Loyanne Monyk Torres Costa
Universidade Federal do Rio Grande do Norte
Santa Cruz - RN, Brasil. CEP 59200-000
Endereço eletrônico: loyannemonyk@hotmail.com
Isabelly Cristina Soares de Oliveira
Facisa/UFRN, Santa Cruz - RN, Brasil. CEP 59200-000
Endereço eletrônico: isaoliveirapsi@gmail.com
Renata Meira Veras
Rua Artur de Sá Menezes, 221 apto 1201, Pituba, Salvador - BA. CEP 41810-480
Endereço eletrônico: renatameiraveras@gmail.com
Recebido em: 15/05/2020
Reformulado em: 02/10/2020
Aceito em: 07/10/2020
Notas
* Psicóloga e Professora do curso de Psicologia da Facisa/UFRN com doutorado em psicologia social. Especialista em psicologia clínica fenomenológica existencial. Trabalha com saúde mental, questões de gênero e clínica psicológica.
** Estudante de Fisioterapia na Universidade Federal do Rio Grande do Norte.
*** Estudante de fisioterapia na Universidade Federal do Rio Grande do Norte.
**** Estudante de Psicologia na Universidade Federal do Rio Grande do Norte.
***** Psicóloga e Fisioterapeuta. Doutora em Psicologia pela Universidade Federal do Rio Grande do Norte. Professora Associada da Universidade Federal da Bahia. Docente Permanente do Programa de Pós-graduação em Psicologia da UFBA. Bolsista Produtividade nível 2 CNPq.
Este artigo de revista Estudos e Pesquisas em Psicologia é licenciado sob uma Licença Creative Commons Atribuição-Não Comercial 3.0 Não Adaptada.














