Services on Demand
article
Indicators
Share
Revista Brasileira de Terapias Cognitivas
Print version ISSN 1808-5687On-line version ISSN 1982-3746
Rev. bras.ter. cogn. vol.17 no.2 Rio de Janeiro July/Dec. 2021
http://dx.doi.org/10.5935/1808-5687.20210023
SYSTEMATIC REVIEW
Effectiveness of Online Cgnitive-Behavioral Therapy in the COVID-19 pandemic scenario: a systematic review
Danilo de Freitas Araújo; Elenkadja Lopes Costa
Faculdade Uninassau Natal/RN, Curso de Psicologia - Natal - Rio Grande do Norte - Brasil
ABSTRACT
The covid-19 pandemic has triggered or aggravated psychiatric symptoms. Thus, cognitive-behavioral interventions online can be viable treatment alternatives. The aim of this systematic review was to describe evidence on the effectiveness of online Cognitive-Behavioral Therapy (CBT) for pandemic-related psychiatric conditions. Randomized clinical trials (RCTs) produced between January 2020 and June 2021 were searched in the PUBMED, LILACS, Web of Science, SCOPUS, Embase and PsycINFO databases, based on the guidelines of the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISM). Seven RCTs were selected and included. The results show that online CBT interventions were effective in decreasing depression, anxiety, dysfunctional concerns, trauma, perceived stress and loneliness, and improving resilience. Three RCTs had a high risk of bias, suggesting the need for further studies, including RCTs and meta-analyses, to improve the strength of the evidence. In conclusion, online CBT has initial evidence of effectiveness in the face of the pandemic scenario.
HEADINGS: Covid-19; Internet-based intervention; Cognitive behavioral therapy.
INTRODUCTION
The emergence of the first confirmed case of the new coronavirus (SARS-CoV-2) brought the alert for what would be classified as a pandemic. The outbreak was first reported in Wuhan, China, on December 31, 2019, according to data from the World Health Organization (WHO),2020, which has also named the disease COVID-19 (Ministry of Health, 2020).
In addition to the serious concerns about the exponential increase in cases, the coronavirus has been producing not only biological and epidemiological repercussions but also social, economic, and emotional impacts (Teotônio et al., 2020). To flatten the epidemic curve, preventive measures were necessary, such as closing restaurants, bars, shops, and schools; as well as the adoption of quarantine and social distancing, causing drastic changes in daily activities (Murphy et al., 2020).
These consequences caused by the pandemic may be greater than the number of deaths, significantly impacting the mental health of individuals (Brooks et al., 2020). The demand for mental health care tends to rise, mainly for those diagnosed with COVID-19, their families, and health workers, due to the risk of death, exposure to the virus, and all the social changes caused by the pandemic (Wind et al., 2020).
A cross-sectional study of 8,079 Chinese adolescents found that 43% presented depressive symptoms, 37% presented anxiety symptoms, and 31% presented a combination of depression and anxiety during the COVID-19 outbreak (Zhou et al., 2020). Other complaints were identified, such as symptoms of post-traumatic stress, confusion, and anger, which may persist in the post-crisis (Brooks et al., 2020).
The management of patients in psychological distress during the pandemic raises considerable questions regarding therapeutic interventions. Different research indicates the existence of a more vulnerable part of the population during the new coronavirus pandemic, suggesting emergency interventions according to the demands presented individually (Kang et al., 2020; Lai et al., 2020; Wu & Wei, 2020).
Thus, the need for evidence-based interventions arises. Cognitive-Behavioral Therapy (CBT) consists of a brief, focused, and collaborative treatment that aims to modify dysfunctional responses, altering the thoughts and behaviors of the individual. It presents a vast number of protocols for treating numerous psychiatric disorders, generally being effective for Obsessive-Compulsive Disorder (OCD), Post Traumatic Stress Disorder (PTSD), Generalized Anxiety Disorder (GAD), and specific phobias (Kaczkurkin & Foa, 2015). In this context, cognitive-behavioral interventions can be viable alternatives to the mental health problems brought by the pandemic.
Considering the situation and growing challenges, there is the need to adapt to an atypical scenario, inserting digital solutions associated with conventional therapy (Di Carlo et al., 2021). The online intervention modality offers greater flexibility in schedules, economy on locomotion, and lower risk of infection (Cowan et al., 2019), in addition to some patients reporting that they feel more open and willing to address difficult issues (Simpson & Reid, 2014).
This new way of intervening in diseases is also reaching the CBT. Its online modality has existed for more than a decade, and initially, this digitization process happened only in the transcription of self-help manuals for websites. Subsequently, three main forms gained space (Luik et al., 2017): online CBT support, in which the therapist provides elements to support conventional therapy; guided online CBT, whose therapy content is explained to the patient with the help of websites and mobile applications with animations, audios, and pictures; and fully automated online CBT, with the patient using the digital tool without any human support (Luik et al., 2019).
The complexity of the current social scenario revisits the importance of investigating and summarizing existing evidence in the literature. Furthermore, there are still scientific gaps regarding the cost and effectiveness of remote care for disorders, requiring the permanent advancement of correlated research (Taylor et al., 2020).
Therefore, it is worth questioning whether remote, synchronous, or asynchronous modalities, based on CBT protocols, could be effective in reducing or eliminating psychological symptoms in different conditions (diagnosed or subsyndromic) that are related to the impacts of COVID-19. And more, if online CBT may be as effective as the conventional one. For these reasons, this literature review has intended to describe the evidence on the effectiveness of this therapy, in the online modality, for psychiatric conditions related to the COVID-19 pandemic.
METHOD
The systematic literature review was performed in four phases: 1) planning the review protocol, starting from the formulation of the problem with the PICOT model (Population, Intervention, Comparator, Outcomes, and Study Categories); 2) systematic search of primary studies and data extraction; 3) critical evaluation of selected studies; 4) and synthesis of the identified evidence; following PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyses) guidelines (Page et al., 2021).
The search was conducted from June 3, 2021, to June 6, of the same year, in the PUBMED and LILACS databases, directly; and in the Web of Science, SCOPUS, PsycINFO, and Embase databases, via CAPES Journals. Both authors independently followed all procedures listed to reduce the risk of bias.
To track publications with a higher degree of sensitivity, combinations between the descriptors DeCS/MeSH and "text words" were used, linked by the Boolean operators "AND" and "OR". Gray literature was not considered. Reference lists of included studies were also checked to identify possible relevant citations.
The following search strategy was formulated for the survey: ("Cognitive Behavioral Therapy"[MeSH Terms] OR "Cognitive Behavioral Therapy Program"[Text Word]) AND (online[MeSH Terms] OR "Online Psychotherapy Tool"[Text Word] OR telemedicine[MeSH Terms] OR teletherapy[Text Word] OR "Internet-Based Intervention"[MeSH Terms] OR "Digital Cognitive Behavioral Therapy"[Text Word] OR "Internet-based cognitive behavioral therapy"[MeSH Terms]) AND ( COVID-19[MeSH Terms] OR "Coronavirus Infections"[MeSH Terms] OR SARS-CoV-2[MeSH Terms] OR Coronavirus[Text Word]).
Complementary searches were performed, between the first one and the moment of extracting the data, to preserve the topicality of the subject. Upon completion, the results were organized with the help of the Mendeley Reference Manager. An initial screening by titles and names of the authors was performed to identify and eliminate duplicates. After this, the inclusion and exclusion criteria were applied.
The inclusion criteria were: 1) randomized controlled trials (RCT); 2) studies that evaluated the effectiveness of online, synchronous, and asynchronous CBT protocols; 3) the ones that had the studied population composed of health workers, individuals hospitalized with COVID-19, or those who were experiencing psychiatric symptoms related to the disease, even without the diagnosis; 4) studies that included the descriptors in the title, abstract and keywords; 5) research published in article format, from January 2020 to June 2021; 6) publications in English and Spanish; and 7) fully accessible texts.
The exclusion criteria were: 1) theoretical articles; 2) studies that did not have CBT as the main component of the intervention; 3) those that did not discuss the effectiveness of CBT for symptoms related to the COVID-19 pandemic; 4) studies that did not address online CBT; 5) and those with participants recruited, selected and randomized before 2020.
Eligible articles were carefully read to facilitate the data extraction process and organized in an Excel spreadsheet after the collection of the name of the authors, year, country, research design, population, inclusion and exclusion criteria, sample size, characterization of the intervention, instruments for outcome assessment, whether there was a follow-up, mean age of the sample and gender distribution, dropout rate throughout the study, results, and primary outcomes. At this stage, each author performed the extraction independently, to achieve 100% consistency of the extracted items. Discrepancies regarding the information were resolved through discussion.
This review also considered the risk of bias for the results of randomized clinical trials, using the Cochrane tool - Cochrane Risk of Bias Tool (Sterne et al., 2019). The domains considered in the process were the participant selection (both randomization and allocation concealment), blinding of participants and care providers, the presence of incomplete outcome data, and selective reporting, in addition to other potential biases. If there were no consensus among the authors, the tool was reapplied until an agreement was reached.
Considering the heterogeneity of the results, which would make statistical analyzes of a meta-analysis difficult, this systematic review chose to present and describe its data written, in text form (Siddaway et al, 2019).
RESULTS
Studies included
From the searches performed (Figure 1),983 results were identified, predominantly found in SCOPUS (939). LILACS did not return results, suggesting the incipience of studies in Latin America about the theme. The same explanation also applies to the absence of research identified in previous reviews.
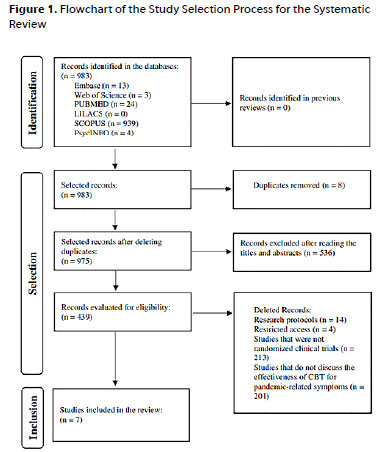
After removing 8 duplicates, 975 studies remained. By reading the titles and abstracts, it was possible to exclude 536 papers that did not meet the purposes of the review, leaving 439.
Other studies were excluded for various reasons, such as being research protocols that will still be operational (14), not allowing full access to the content (4), not having a randomized clinical trial design (213), and not addressing the effectiveness of CBT for psychiatric conditions related to the COVID-19 pandemic (201). Therefore, the final sample consisted of 7 randomized controlled trials on the effectiveness of online Cognitive Behavior Therapy for pandemic-related psychiatric symptoms.
Characteristics of the studies
All of the retrieved papers were published between November 2020 and May 2021. Following the defined inclusion criteria, all eligible studies were randomized clinical trials. However, some peculiarities are highlighted (Table 1). Only one of them was conducted in 2020 (Wahlund et al., 2020). Three of them were conducted in Middle Eastern countries (Al-Alawi et al., 2021; Shapira et al., 2021; Shaygan et al., 2021), three on the European continent (Perri et al., 2021; Preuss et al., 2021; Wahlund et al., 2020) and one in Asia (Liu et al., 2021).
Eligible samples had a wide range of variations, with some involving 38 subjects (Perri et al., 2021), and others with 670 (Wahlund et al., 2020). The dropout rates of participants ranged from 10 to 38%, between the pre- and post-intervention moments.
The study outcomes were quite heterogeneous. In the studies by Al-Alawi et al. (2021) and Liu et al. (2021), anxiety and depression were the primary outcomes analyzed; depression, combined with loneliness, were evaluated in the study by Shapira et al. (2021); and dysfunctional concerns (an important component for understanding anxiogenic conditions) were analyzed in the protocol by Wahlund et al. (2020). The instruments were mostly scales and questionnaires, such as the GAD-7 (Al-Alawi et al., 2021; Wahlund et al., 2020) and the PHQ-9 (Al-Alawi et al., 2021; Shapira et al., 2021), used to measure the outcomes in two protocols, each.
All interventions evaluated were mostly based on Cognitive Behavioral Therapy, however, only Perri et al. (2021) and Wahlund et al. (2020) focused on cognitive restructuring and problem-solving. Three other clinical trials incorporated elements of mindfulness and meditation into cognitive-behavioral strategies (Liu et al., 2021; Shapira et al., 2021; Shaygan et al., 2021).
Furthermore, only two interventions were guided by trained health professionals, synchronously; one of them is similar to a brief individual therapeutic process (Al-Alawi et al., 2021), and the other as group therapy (Shapira et al., 2021). The others were structured as asynchronous and self-guided online intervention programs.
Effectiveness of the interventions studied in randomized clinical trials
All seven RCTs showed a statistically significant reduction in outcomes in the groups that received the intervention. Except for Shaygan et al. (2021), whose results revealed a significant improvement in the resilience outcome. Liu et al. (2021), Perri et al. (2021), and Wahlund et al. (2020) evaluated the follow-up one month after the end of the interventions, suggesting maintenance of the effects.
It was also possible to verify significant results in the measurements of secondary outcomes, comparing the intervention group and the control one, regarding the pre- and post-intervention moments. Improvements were seen in insomnia, mood, daily functioning, uncertainty intolerance (Wahlund et al., 2020; Liu et al., 2021); perceived stress (Shaygan et al., 2021); and negative affective symptoms (Preuss et al., 2021).
Risk of bias
As recommended by the Cochrane Collaboration, the Cochrane Risk of Bias Tool was used, which classifies the risk of bias as high, low, or unclear. Of the seven studies included (Table 2), four of them presented low risk (Wahlund et al., 2020; Preuss et al., 2021; Shaygan et al., 2021; Al-Alawi et al., 2021), and the other three, high risk (Perri et al., 2021; Liu et al., 2021; Shapira et al., 2021).
As for specific domains, the study by Liu et al. (2021) presented a high risk of bias due to the absence of blinding of participants and care workers (the participants, all diagnosed with mild COVID-19, were recruited from five hospitals, which made it impossible for the research team to approach the implementation of blinding measures). The article by Shapira et al. (2021) did not present all outcome data (does not mention exclusion criteria for sample selection, and frequencies distributed by gender are not specified).
Some methodological concerns arise from the analysis of biases in some of the studies, especially when there is no satisfactory detail for a critical judgment to be performed. In one of them, this occurs in at least four domains (Shapira et al., 2021), including blinding of participants and researchers, blinding of outcome assessor, and selective reporting. In another one, it occurs in all domains (Perri et al., 2021), suggesting a lack of sufficient data to assess the presence of an important risk of bias. The presence of risk in several, or in all domains, is a strong indication that there is a bias capable of influencing research results.
A study likely to be biased may have several categories of methodological flaws or omissions. For example, Perri et al. (2021) comparatively evaluate two interventions, and for this, one group is submitted to online CBT, and the other to EMDR (Eye Movement Desensitization and Reprocessing) therapy. The absence of a control condition that submits part of the participants to the waiting list or a usual intervention also indicates a high risk of bias. In addition, the authors do not specify exclusion criteria and do not inform the dropout rate of the participants.
Discussion
Since the beginning of 2020, the world has been experiencing one of the most critical moments in recent decades. Amid a context in which world health agencies rethink intervention models, this systematic literature review has aimed to survey the state-of-the-art on online Cognitive Behavior Therapy for psychic conditions related to political, economic, social, and psychological repercussions of the COVID-19 pandemic.
It must be remembered that, in the coming years, a progressive increase in emotional problems resulting from this event is expected. Preliminary evidence even suggests that symptoms of anxiety and depression (16% to 28% prevalence) and perceived stress (8%) are common psychological reactions, in addition to being associated with sleep disturbances (Rajkumar, 2020). Several data from recent literature have also confirmed immediate and potentially long-term negative effects on the mental health of nurses (Chew et al., 2020), physicians, and the general medical team (Lu et al., 2020).
Significant evidence was found, in this review, about the effectiveness of online Cognitive-Behavioral Therapy interventions to treat emotional disorders that the pandemic has brought to people. This can be considered an important new finding, even more so that CBT (online and mediated by a trained healthcare professional, or through digital applications and software) has positive acceptance among patients and produces results similar to therapy in-person (Stubbings et al., 2013).
All seven randomized clinical trials retrieved show effectiveness results comparable to conventional CBT, for individuals who experienced psychological distress during the pandemic. Similarly, Pandey et al. (2020) found a significant reduction in the levels of anxiety, depression, and stress in a group of Chinese patients who tested positive for COVID-19, and who underwent a CBT protocol, compared to the group in the routine treatment, following the guidelines for managing the same disease.
In the present literature review, the evidence supported by a larger number of studies is that stress, anxiety, depression, and dysfunctional concerns - some of the most recurrent psychiatric conditions in the pandemic period - are significantly reduced with online CBT. These findings are similar to those by Ebert et al. (2015) and Rose et al. (2013), on the effectiveness of conventional CBT protocols for depressive, anxiogenic, and stress conditions.
Online CBT, considering the evidence, helps individuals to more logically and rationally assess the anticipatory and catastrophic concerns experienced, to deal with stressors that exacerbate symptoms (for example, news about the increase in the number of confirmed cases of the disease and deaths), as well as contributing to the improvement of mindfulness of the body, mind, and environmental stimuli. The set of such interventions usually make up most evidence-based CBT protocols (Hofmann et al., 2012).
Posttraumatic Stress Disorder (PTSD) is also a condition that can be a consequence of the pandemic context, affecting frontline health workers who deal with life and death issues daily, survivors who contracted more severe forms of Sars-CoV-2, in addition to people grieving the loss of family, friends, and acquaintances. This review also identified the benefits of online CBT for trauma resulting from the pandemic, in agreement with the randomized clinical trial by Kredlow et al. (2017) on the effectiveness of CBT for PTSD.
Remote interventions can be important for patients who have difficulty exposing themselves to aversive situations, something very common in PTSD. Cognitive restructuring of CBT, applied to dysfunctional trauma, helps in tracking and altering generalized maladaptive cognitions that make it difficult to confront the traumatic reality, and that maintain negative emotions (notably guilt) and useless coping behaviors (Klein et al., 2010).
Since the present review suggests the effectiveness of online CBT for a wide range of outcomes, it is possible to make assumptions about possible applications for other clinical settings. Online interventions are already discussed, or supported by evidence, in recent studies on grief (Boelen et al., 2021), Obsessive-Compulsive Disorder (Seoul et al., 2016), and social anxiety (Nordgreen et al., 2018). There are precedents for these disorders to be studied taking into consideration the stressors from the pandemic.
Despite the promising results, three of the retrieved studies had low methodological quality. They lack a control group, double-blinding in the randomization of the sample, and do not include a satisfactory discussion of the data in outcome reporting. Such indicators, when not met, can bias the results of a survey, weakening the evidence, in addition to being biased in favor of digital tools. Therefore, they must be carefully evaluated.
On the other hand, most of the included studies were of good quality, and the results are encouraging, in terms of the effectiveness of online CBT for users of mental health services with diverse diagnoses. They can constitute a robust and consistent source of information for managers, public policies in mental health, and other decision-makers.
As for the limitations, it is worth mentioning, specifically, the small number of studies involving online CBT and the psychological effects of the pandemic. Many protocols for new RCTs are in the early stages of implementation, requiring periodic systematic reviews, providing evidence that they are feasible in the long term. Another limitation is the absence of quantifiable measures for summarizing the results. It is argued, however, that the option for textual synthesis was due to methodological heterogeneity and the findings of the studies, which can also be circumvented in future reviews that retrieve a larger number of RCTs.
CONCLUSION
From the data collected, analyzed, and summarized on online Cognitive-Behavioral Therapy during the COVID-19 pandemic, it was possible to verify its effectiveness for psychiatric symptoms. This is important evidence for planning interventional actions to promote mental health.
It is noteworthy that, although the present study has achieved its objective, it did not have the ambition to exhaust the topic or definitively answer any question regarding online CBT and its effectiveness.
Further research can focus on 1) performing meta-analyses that introduce statistical measures, and improve the robustness of evidence; 2) proposing RCTs that perform direct comparisons between conventional and online CBT interventions during the pandemic and its aftermath; and 3) considering other psychiatric conditions whose incidence has increased due to COVID-19.
REFERENCES
Al-Alawi, M., McCall, R. K., Sultan, A., Al Balushi, N., Al-Mahrouqi, T., Al Ghailani, A., ... Al Sinawi, H. (2021). Efficacy of a six-week-long therapist-guided online therapy versus self-help internet-based therapy for COVID-19-induced anxiety and depression: Open-label, pragmatic, randomized controlled trial. JMIR Mental Health, 8(2),e26683. https://doi.org/10.2196/26683 [ Links ]
Boelen, P. A., Eisma, M. C., Smid, G. E., de Keijser, J., & Lenferink, L. I. M. (2021). Remotely delivered cognitive behavior therapy for disturbed grief during the COVID-19 crisis: Challenges and opportunities. Journal of Loss & Trauma, 26(3),211-219. https://doi.org/10.1080/15325024.2020.1793547 [ Links ]
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395(10227),912-920. https://doi.org/10.1016/S0140-6736(20)30460-8 [ Links ]
Chew, N. W. S., Lee, G. K. H., Tan, B. Y. Q., Jing, M., Goh, Y., Ngiam, N. J. H., ... Sharma, V. K. (2020). A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain, Behavior, and Immunity, 88,559-565. https://doi.org/10.1016/j.bbi.2020.04.049 [ Links ]
Cowan, K. E., McKean, A. J., Gentry, M. T., & Hilty, D. M. (2019). Barriers to use of telepsychiatry: Clinicians as gatekeepers. Mayo Clinic Proceedings, 94(12),2510-2523. https://doi.org10.1016/j.mayocp.2019.04.018 [ Links ]
Di Carlo, F., Sociali, A., Picutti, E., Pettorruso, M., Vellante, F., Verrastro, V., ... di Giannantonio, M. (2021). Telepsychiatry and other cutting-edge technologies in COVID-19 pandemic: Bridging the distance in mental health assistance. International Journal of Clinical Practice, 75(1),e13716. https://doi.org/10.1111/ijcp.13716 [ Links ]
Ebert, D. D., Zarski, A.-C., Christensen, H., Stikkelbroek, Y., Cuijpers, P., Berking, M., & Riper, H. (2015). Internet and Computer-Based Cognitive Behavioral Therapy for anxiety and depression in youth: A meta-analysis of randomized controlled outcome trials. PLoS ONE, 10(3),e0119895. https://doi.org/10.1371/journal.pone.0119895 [ Links ]
Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of Cognitive Behavioral Therapy: A review of meta-analyses. Cognitive Therapy and Research, 36(5),427-440. https://doi.org/10.1007/s10608-012-9476-1 [ Links ]
Kaczkurkin, A. N., & Foa, E. B. (2015). Cognitive-behavioral therapy for anxiety disorders: An update on the empirical evidence. Dialogues in clinical neuroscience, 17(3),337-346. https://doi.org/10.31887/DCNS.2015.17.3/akaczkurkin [ Links ]
Kang, L., Ma, S., Chen, M., Yang, J., Wang, Y., Li, R., ... Liu, Z. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain, behavior, and immunity, 87,11-17. https://doi.org/10.1016/j.bbi.2020.03.028 [ Links ]
Klein, B., Mitchell, J., Abbott, J., Shandley, K., Austin, D., Gilson, K., ... Redman, T. (2010). A therapist-assisted cognitive behavior therapy internet intervention for posttraumatic stress disorder: Pre-, post- and 3-month follow-up results from an open trial. Journal of Anxiety Disorders, 24(6),635-644. https://doi.org/10.1016/J.JANXDIS.2010.04.005 [ Links ]
Kredlow, M. A., Szuhany, K. L., Lo, S., Xie, H., Gottlieb, J. D., Rosenberg, S. D., & Mueser, K. T. (2017). Cognitive behavioral therapy for posttraumatic stress disorder in individuals with severe mental illness and borderline personality disorder. Psychiatry Research, 249,86-93. https://doi.org/10.1016/j.psychres.2016.12.045 [ Links ]
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., ... Hu, S. (2020). Factors associated with mental health outcomes among health care workers exposed to Coronavirus Disease 2019. JAMA Network Open, 3(3),e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976 [ Links ]
Liu, Z., Qiao, D., Xu, Y., Zhao, W., Yang, Y., Wen, D., ... Xu, Y. (2021). The efficacy of computerized cognitive behavioral therapy for depressive and anxiety symptoms in patients with COVID-19: Randomized controlled trial. Journal of Medical Internet Research, 23(5),e26883. https://doi.org/10.2196/26883 [ Links ]
Lu, W., Wang, H., Lin, Y., & Li, L. (2020). Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Research, 288,112936. https://doi.org/10.1016/j.psychres.2020.112936 [ Links ]
Luik, A. I., Kyle, S. D., & Espie, C. A. (2017). Digital Cognitive Behavioral Therapy (dCBT) for Insomnia: A state-of-the-science review. Current Sleep Medicine Reports, 3(2),48-56. https://doi.org/10.1007/s40675-017-0065-4 [ Links ]
Luik, A. I., van der Zweerde, T., van Straten, A., & Lancee, J. (2019). Digital delivery of Cognitive Behavioral Therapy for Insomnia. Current Psychiatry Reports, 21(7),50. https://doi.org/10.1007/s11920-019-1041-0. [ Links ]
Ministério da Saúde (2020). Protocolo de manejo clínico para o novo-coronavírus (2019-nCoV). https://portalarquivos2.saude.gov.br/images/pdf/2020/fevereiro/11/protocolo-manejo-coronavirus.pdf. [ Links ]
Murphy, R., Calugi, S., Cooper, Z., & Dalle Grave, R. (2020). Challenges and opportunities for enhanced cognitive behaviour therapy (CBT-E) in light of COVID-19. The Cognitive Behaviour Therapist, 13, E14. doi: 10.1017/S1754470X20000161 [ Links ]
Nordgreen, T., Gjestad, R., Andersson, G., Carlbring, P., & Havik, O. E. (2018). The effectiveness of guided internet-based cognitive behavioral therapy for social anxiety disorder in a routine care setting. Internet Interventions, 13,24-29. https://doi.org/10.1016/j.invent.2018.05.003 [ Links ]
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., ... Moher, D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ, 372, n71. https://doi.org/10.1136/bmj.n71 [ Links ]
Pandey, R., Ramachandran, P., Li, J., Li, X., Jiang, J., Xu, X., Wu, J., Xu, Y., Lin, X., Hall, J., Xu, H., Xu, J., & Xu, X. (2020). The Effect of Cognitive Behavioral Therapy on depression, anxiety, and stress in patients with COVID-19: A randomized controlled trial. Frontiers in Psychiatry, 11,1096. https://doi.org/10.3389/fpsyt.2020.580827 [ Links ]
Perri, R. L., Castelli, P., La Rosa, C., Zucchi, T., & Onofri, A. (2021). COVID-19, isolation, quarantine: On the efficacy of internet-based eye movement desensitization and reprocessing (EMDR) and cognitive-behavioral therapy (CBT) for ongoing trauma. Brain Sciences, 11(5),579. https://doi.org/10.3390/brainsci11050579 [ Links ]
Preuss, H., Capito, K., van Eickels, R. L., Zemp, M., & Kolar, D. R. (2021). Cognitive reappraisal and self-compassion as emotion regulation strategies for parents during COVID-19: An online randomized controlled trial. Internet Interventions, 24,100388. https://doi.org/10.1016/j.invent.2021.100388 [ Links ]
Rajkumar, R. P. (2020). COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52,102066. https://doi.org/10.1016/j.ajp.2020.102066 [ Links ]
Rose, R. D., Buckey, J. C., Zbozinek, T. D., Motivala, S. J., Glenn, D. E., Cartreine, J. A., & Craske, M. G. (2013). A randomized controlled trial of a self-guided, multimedia, stress management and resilience training program. Behaviour Research and Therapy, 51(2),106-112. https://doi.org/10.1016/j.brat.2012.11.003 [ Links ]
Seol, S.-H., Kwon, J. S., Kim, Y. Y., Kim, S. N., & Shin, M.-S. (2016). Internet-Based Cognitive Behavioral Therapy for Obsessive-Compulsive Disorder in Korea. Psychiatry Investig, 13(4),373-382. https://doi.org/10.4306/pi.2016.13.4.373 [ Links ]
Shapira, S., Yeshua-Katz, D., Cohn-Schwartz, E., Aharonson-Daniel, L., Sarid, O., & Clarfield, A. M. (2021). A pilot randomized controlled trial of a group intervention via Zoom to relieve loneliness and depressive symptoms among older persons during the COVID-19 outbreak. Internet Interventions, 24, 100368. https://doi.org/10.1016/j.invent.2021.100368 [ Links ]
Shaygan, M., Yazdani, Z., & Valibeygi, A. (2021). The effect of online multimedia psychoeducational interventions on the resilience and perceived stress of hospitalized patients with COVID-19: A pilot cluster randomized parallel-controlled trial. BMC Psychiatry, 21(1). https://doi.org/10.1186/s12888-021-03085-6 [ Links ]
Siddaway, A. P., Wood, A. M., & Hedges, L. V. (2019). How to do a systematic review: A best practice guide for conducting and reporting narrative reviews, meta-analyses, and meta-syntheses. Annual Review of Psychology, 70(1),747-770. https://doi.org/10.1146/annurev-psych-010418-102803 [ Links ]
Simpson, S. G., & Reid, C. L. (2014). Therapeutic alliance in videoconferencing psychotherapy: A review. Australian Journal of Rural Health, 22(6),280-299. https://doi.org/10.1111/ajr.12149 [ Links ]
Sterne, J. A. C., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., ... Higgins, J. P. T. (2019). RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ,366, l4898. https//doi.org/10.1136/bmj.l4898. PMID: 31462531 [ Links ]
Stubbings, D. R., Rees, C. S., Roberts, L. D., & Kane, R. T. (2013). Comparing in-person to Videoconference-Based Cognitive Behavioral Therapy for mood and anxiety disorders: Randomized controlled trial. Journal of Medical Internet Research, 15(11),e258. https://doi.org/10.2196/jmir.2564 [ Links ]
Taylor, C. B., Fitzsimmons-Craft, E. E., & Graham, A. K. (2020). Digital technology can revolutionize mental health services delivery: The COVID-19 crisis as a catalyst for change. The International Journal of Eating Disorders, 53(7),1155-1157. https://doi.org/10.1002/eat.23300 [ Links ]
Teotônio, I., Hecht, M., Castro, L. C., Gandolfi, L., Pratesi, R., Nakano, E. Y., ... Pratesi, C. B. (2020). Repercussion of COVID-19 pandemic on Brazilians' quality of life: A nationwide cross-sectional study. International Journal of Environmental Research and Public Health, 17(22),8554. https://doi.org/10.3390/ijerph17228554 [ Links ]
Wahlund, T., Mataix-Cols, D., Olofsdotter Lauri, K., De Schipper, E., Ljótsson, B., Aspvall, K., & Andersson, E. (2021). Brief online cognitive behavioural intervention for dysfunctional worry related to the COVID-19 pandemic: A randomised controlled trial. Psychotherapy and Psychosomatics, 90(3),191-199. https://doi.org/10.1159/000512843 [ Links ]
Wind, T. R., Rijkeboer, M., Andersson, G., & Riper, H. (2020). The COVID-19 pandemic: The 'black swan' for mental health care and a turning point for e-health. Internet Interventions, 20,100317. https://doi.org/10.1016/j.invent.2020.100317 [ Links ]
World Health Organization (WHO) (2020). Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [ Links ]
Wu, K., & Wei, X. (2020). Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China. Medical Science Monitor Basic Research, 26, e924085. https://doi.org/10.12659/MSMBR.924085 [ Links ]
Zhou, S. J., Zhang, L. G., Wang, L. L., Guo, Z. C., Wang, J. Q., Chen, J. C., ... Chen, J. X. (2020). Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. European Child & Adolescent Psychiatry, 29(6),749-758. https://doi.org/10.1007/s00787-020-01541-4 [ Links ]
 Correspondence:
Correspondence:
Danilo de Freitas Araújo
E-mail: danilodefreitas_1@hotmail.com
Este artigo foi submetido no SGP (Sistema de Gestão de Publicações) da RBTC em 27 de Julho de 2021. cod. 230
Artigo aceito em 15 de Outubro de 2021











 text in
text in 


